The Price of Cold Ischemia Time
1JHU, Baltimore, MD, 2Surgery, University of Maryland, Baltimore, MD
Meeting: 2022 American Transplant Congress
Abstract number: 205
Keywords: Kidney
Topic: Clinical Science » Kidney » 32 - Kidney Deceased Donor Selection
Session Information
Session Name: Kidney Deceased Donor Selection I
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:40pm-4:50pm
Presentation Time: 4:40pm-4:50pm
Location: Hynes Ballroom C
*Purpose: Recent allocation policy changes for deceased-donor kidney transplantation (DDKT) have favored geographic equity over local allocation. Increasing travel distance has the potential to increase cold ischemia time (CIT). Understanding the potential costs to increased CIT in terms of delayed graft function (DGF), use of thymoglobulin for induction, hospital length-of-stay (LOS), and long-term graft survival is critical to understand the tradeoffs involved.
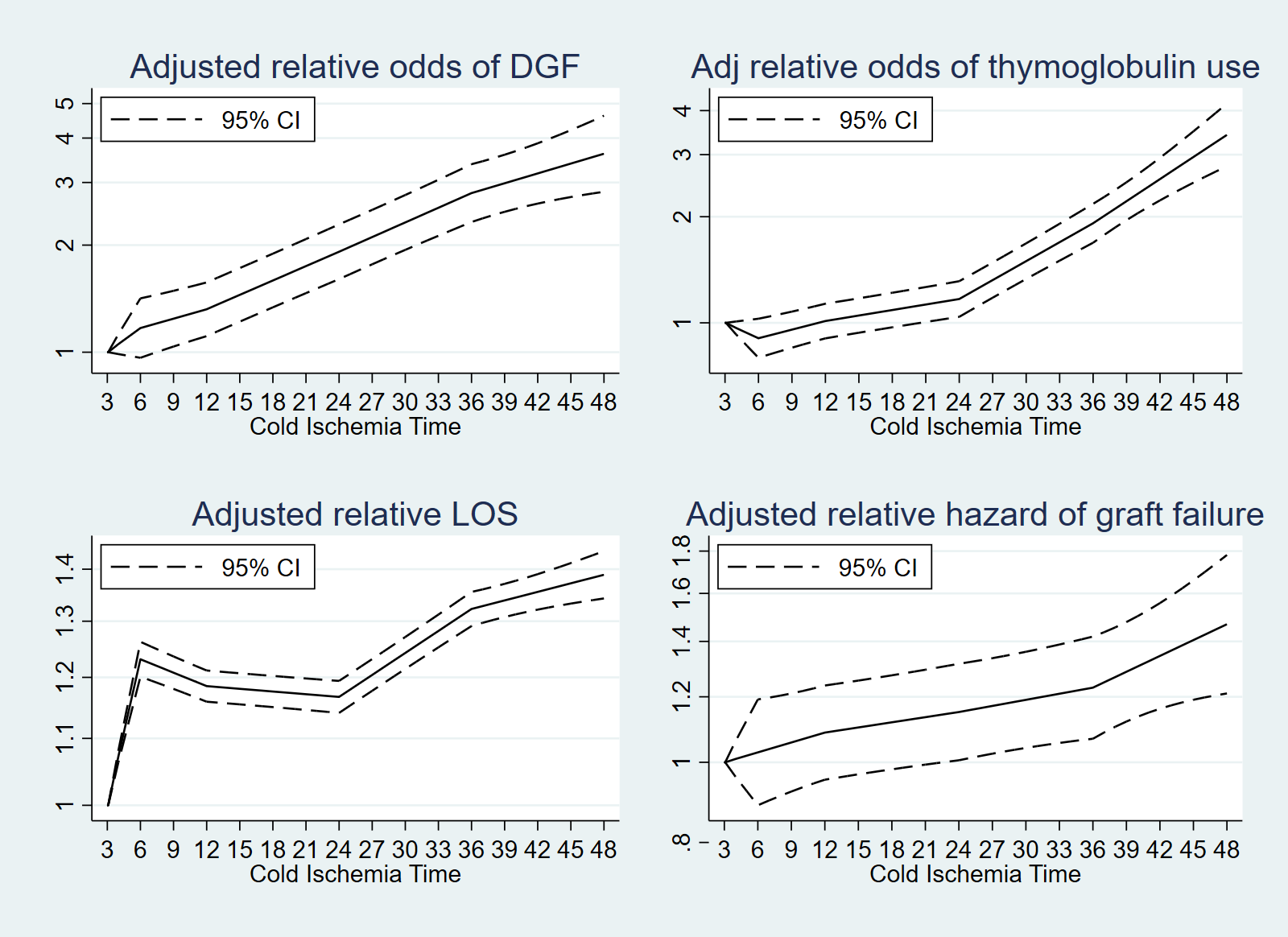
*Methods: Using SRTR data on kidney-only DDKT recipients 2011-2020 with followup through June 2021, we modeled the association between CIT and risk of DGF using multilevel logistic regression adjusting for donor, recipient, and transplant characteristics. CIT was modeled with splines at 6, 12, 24, and 36 hours. Similarly, we modeled the association between CIT and thymoglobulin induction using multivariable logistic regression, LOS using Poisson regression, and graft survival using Cox regression.
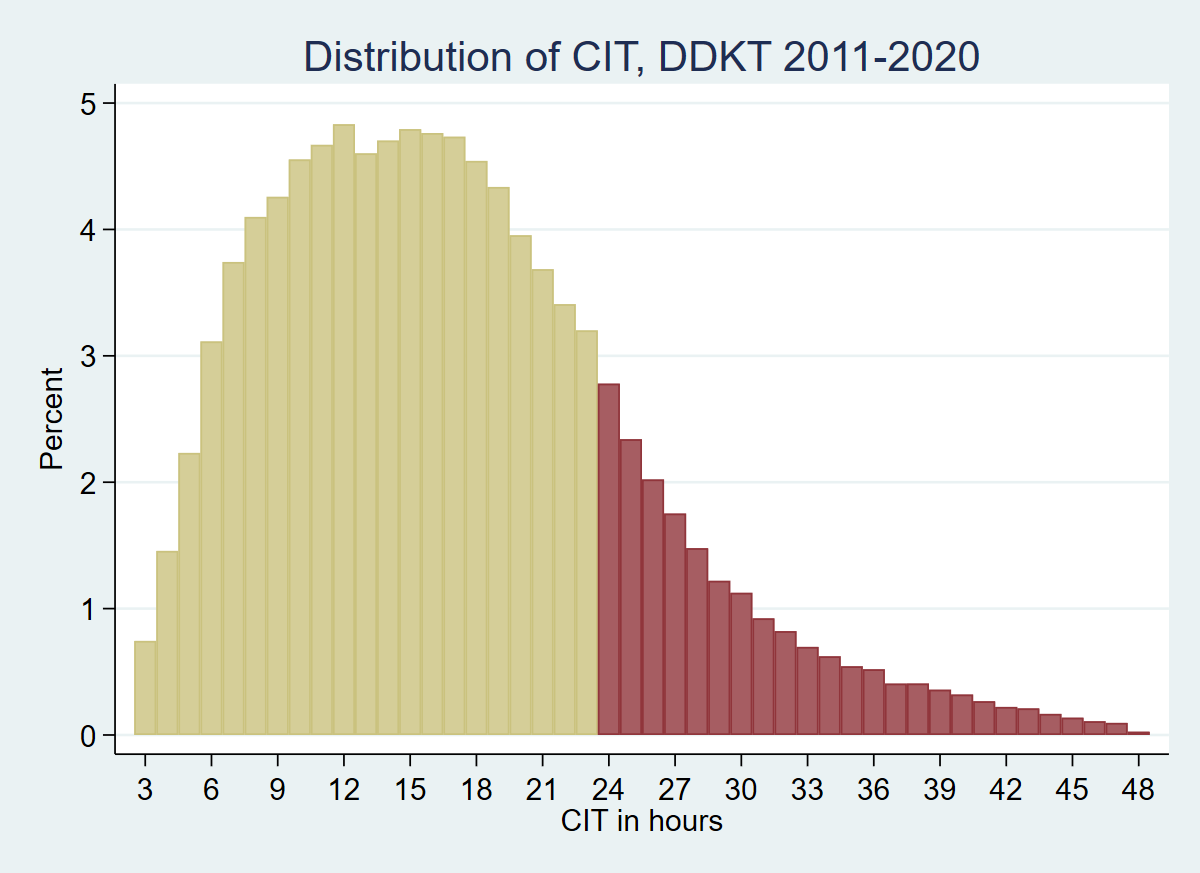
*Results: Among 130,556 DDKT recipients, median (IQR) CIT was 16.3 (11.0-22.2) hours (Figure); CIT was ≥24h for 19.6% of recipients. CIT increased from 15.6 (10.7-21.6)h in 2011 to 17.3 (11.9-22.7)h in 2019 and 17.1 (11.6-22.7)h in 2020. 27.4% of recipients experienced DGF. In adjusted models, each hour of CIT was associated with a 5% increase in DGF risk (hours 3-6) and with a 2.1%-3.2% increase in DGF risk thereafter (Figure 2). The CIT/DGF association was the same for DBD and DCD KT (interaction p=0.94) and consistent over time (interaction p for pre/post-2017=0.53). Interaction with donor age was borderline significant (p=0.054 for age<40 vs age 40+), but small in magnitude (5% difference in odds for 20h of CIT). Compared to CIT=3h, CIT=6h was associated with 23% longer LOS; CIT=36h was associated with 32% longer LOS (figure). CIT ≥24h was associated with substantially increased odds of thymoglobulin at induction and increased risk of graft failure (Figure 2).
*Conclusions: CIT for most DDKT in the United States substantially exceeds the time required even for cross-country travel. CIT contributes to substantial resource burden for transplant centers, and worse short-term and long-term outcomes. The transplant community must strive to reduce CIT in all aspects of organ allocation and distribution, without sacrificing geographic fairness.
To cite this abstract in AMA style:
Massie A, Scalea J, Segev D. The Price of Cold Ischemia Time [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/the-price-of-cold-ischemia-time/. Accessed February 17, 2026.« Back to 2022 American Transplant Congress