The Living Donor Collective Pilot Evaluations of Living Liver Donor Candidates at 6 Programs
B. Kasiske, M. Conboy, Y. Ahn, A. Israni, J. Snyder
SRTR, Minneapolis, MN
Meeting: 2020 American Transplant Congress
Abstract number: C-151
Keywords: Donation, Donors, unrelated, Patient education, Survival
Session Information
Session Name: Poster Session C: Liver: Living Donors and Partial Grafts
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Much remains to learn regarding the long-term effects of living organ donation on donors. Rare events are important, and long-term follow-up with appropriate contemporaneous controls is needed. SRTR, under contract with the Health Resources and Services Administration, is conducting a pilot program to establish a registry of living donor candidates, the Living Donor Collective (LDC).
*Methods: We invited 6 living liver donor programs to participate in the LDC pilot phase. Donor candidates who come prescreened to the transplant program for evaluation are registered with online or batch upload of data submitted to SRTR. After a maximum of 6 months, donation acceptance or reason(s) for not donating are submitted.
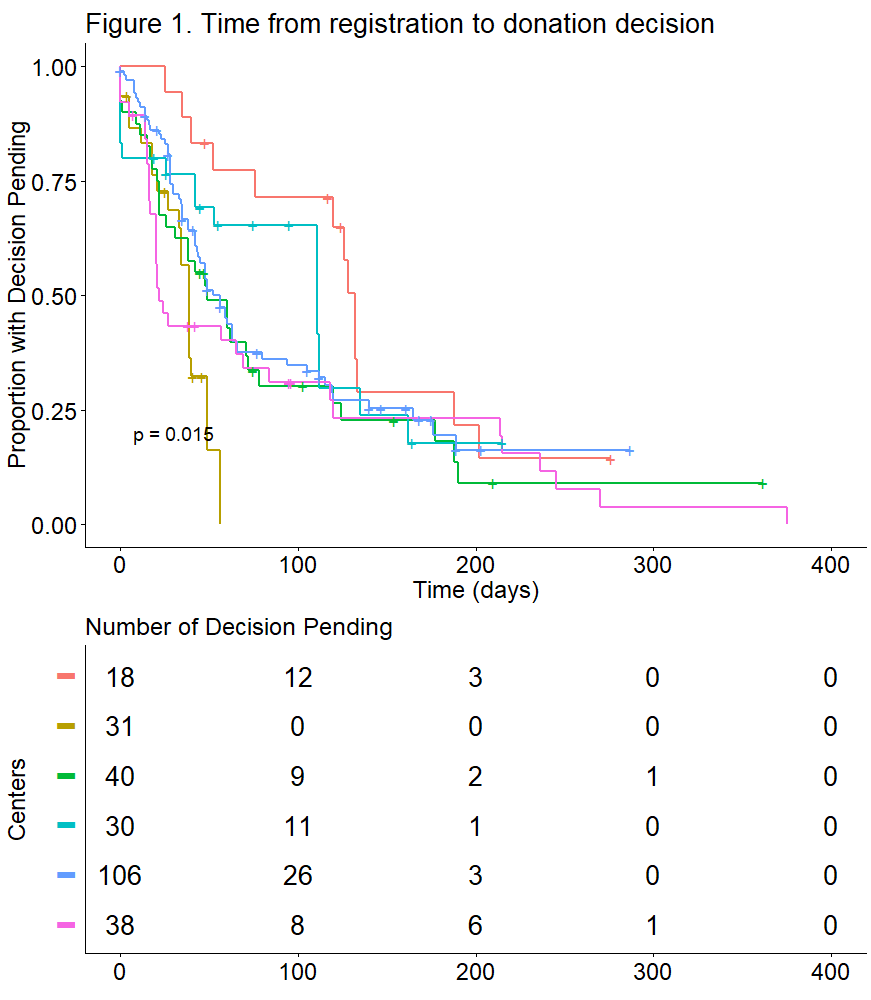
*Results: The first liver donor candidates registered at the first pilot site in May 2018. By Sept 30, 2019, all 6 pilot LDC sites were operational, with a total of 256 candidates: 256/258 (99.2%) completed registration; 182/256 (71.1%) received a determination; and 78/182 (42.9%) were approved to donate. Across all sites, the median days from donor candidate registration to donation approval or decision not to donate was 56 (Fig. 1), with significant variation by program from a minimum of 22 to a maximum of 132 days, log rank P=0.015.
Of 104 donor candidates who did not donate, the most common donor-related reasons were inadequate liver volume on imaging, vascular or biliary abnormalities, other unfavorable anatomic abnormalities, evidence of liver disease, other biopsy abnormalities, obesity, multiple psychosocial stressors, and psychiatric illness; 30 (29%) did not donate because the donation became unnecessary for reasons related only to the intended recipient. The latter could serve as optimal controls for long-term follow-up studies.
*Conclusions: We conclude that establishing a registry of living liver donor candidates is feasible. Reporting the outcomes of donor candidate evaluations to transplant programs, compared other programs, may help programs better understand their candidate evaluation processes. Long-term follow-up of donors and donor candidates who did not donate may provide much needed information on important outcomes, and may facilitate the donation process in the future.
To cite this abstract in AMA style:
Kasiske B, Conboy M, Ahn Y, Israni A, Snyder J. The Living Donor Collective Pilot Evaluations of Living Liver Donor Candidates at 6 Programs [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-living-donor-collective-pilot-evaluations-of-living-liver-donor-candidates-at-6-programs/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress