The Impact of Eplet Mismatches on Kidney Transplant Outcome: A Single-Center Cohort Study
1Department of Microbiology and Immunology, KU Leuven, Leuven, Belgium, 2Histocompatibility and Immunogenetics Laboratory, Belgian Red Cross-Flanders, Mechelen, Belgium, 3University Hospitals Leuven, Leuven, Belgium
Meeting: 2019 American Transplant Congress
Abstract number: A206
Keywords: Allocation, Epitopes, HLA matching, Kidney transplantation
Session Information
Session Name: Poster Session A: Kidney Deceased Donor Allocation
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: It has been shown that HLA-matching at classic antigen-level for HLA-A, -B and -DRB1 loci, provides benefits in matching and outcome after solid organ transplantation. However, despite the significant progress made in the field with new technologies and more potent immunosuppressive agents, long-term graft survival in solid organ transplantation remains impaired. Evaluating HLA eplet mismatches (MM) instead of antigen mismatches could theoretically enable better assessment of the donor-recipient HLA incompatibility and provide better outcome prediction. Due to the need of high-resolution genotyping, studies on this topic are limited, by lower sample sizes or incomplete genotyping. Therefore, in this study, we aimed to evaluate the impact of the eplet mismatches on kidney transplant outcome in a large cohort of donor-recipient pairs with full HLA genotyping at high-resolution level.
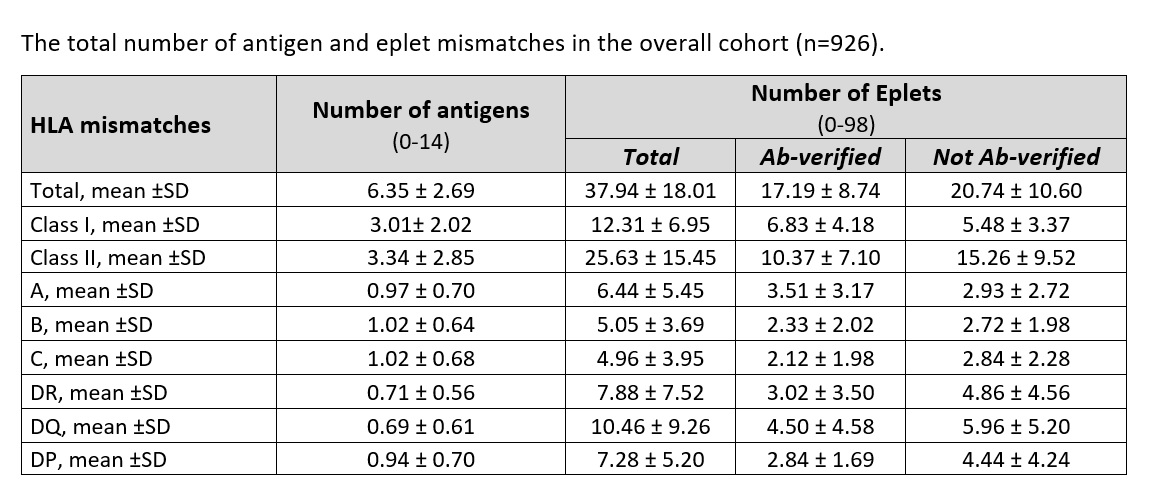
*Methods: All consecutive adult kidney recipients transplanted at a single center between March 2004 and February 2013 were included in this study. In total, 926 transplant pairs were retrospectively genotyped at high resolution by Antigen Recognition Site (ARS) typing of exon 2, 3 and 4 for class I (HLA -A, -B and -C) and exon 2 and 3 for class II (HLA-DRB1, -DRB3, -DRB4, -DRB5, -DQA1, -DQB1, -DPA1, and -DPB1). HLAMatchmaker software was used to determinate the total number of HLA epitope/eplet MM for each transplant pair. Two groups of eplet MM, eplets of the antibody-verified epitopes and predicted eplets as potential epitopes but not yet antibody-verified, were calculated for all HLA loci together, for HLA class I and class II separately, as well as for each locus separately.
*Results: Our study cohort comprised mainly first single-kidney transplant recipients (86.7%) with mean age of 53.8 ±13.2 years, male (59.8%) and mainly Caucasians (98.4%). Pretransplant donor-specific HLA antibodies were present in 10.2% of the recipients, all with a negative CDC crossmatch. Total HLA antigen mismatches ranged from 0 to 14, while the total number of HLA eplet mismatches ranged from 0 to 98. At the level of the individual HLA molecules, the highest mean of antigen mismatches was observed for the B molecule, while the highest number of eplet mismatches was observed for the DQ molecule. Univariate and multivariate Cox analyses confirmed that the classical HLA-A, -B and-DR antigen mismatches were significantly associated with graft failure. Considering the eplet mismatches, the total number of eplet mismatches was not associated with increased risk of graft failure, and only weak associations were found with class II antibody-verified epitope mismatches, likely explained exclusively by the antibody-verified eplet mismatches in the HLA-DQ locus. The subsequent multivariate Cox model, adjusted for the other baseline variables including the presence of pretransplant HLA antibodies, confirmed that antibody-verified DQ epitope mismatches and classical HLA-A,-B and-DR antigen mismatches are both associated with the highest risk of graft failure. Nevertheless, the number of eplet mismatches did not provide better risk prediction than antigen mismatch analysis.
*Conclusions: In conclusion, our results show that the total number of eplet mismatches will not offer better prediction of graft outcome compared to the classical antigen mismatches.
To cite this abstract in AMA style:
Senev A, Coemans M, Sandt VVan, Sprangers B, Kuypers D, Emonds M, Naesens M. The Impact of Eplet Mismatches on Kidney Transplant Outcome: A Single-Center Cohort Study [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-eplet-mismatches-on-kidney-transplant-outcome-a-single-center-cohort-study/. Accessed February 21, 2026.« Back to 2019 American Transplant Congress