The Effect of the Affordable Care Act on Insurance Status, Waitlist, and Transplant Outcomes in Liver Transplantation
1Surgery, Duke University, Durham, NC, 2Population Health Sciences, Duke University, Durham, NC, 3Biostatistics, Duke University, Durham, NC
Meeting: 2021 American Transplant Congress
Abstract number: 114
Keywords: Kidney transplantation, Outcome
Topic: Clinical Science » Biomarkers, Immune Assessment and Clinical Outcomes
Session Information
Session Name: Biomarkers, Immune Assessment and Clinical Outcomes - II
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 6, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 4:45pm-4:50pm
Presentation Time: 4:45pm-4:50pm
Location: Virtual
*Purpose: The Affordable Care Act (ACA) intended to expand Medicaid to cover all adults with income below 138% of federal poverty level. We describe the effect of the ACA on payor status and outcomes of liver transplant candidates.
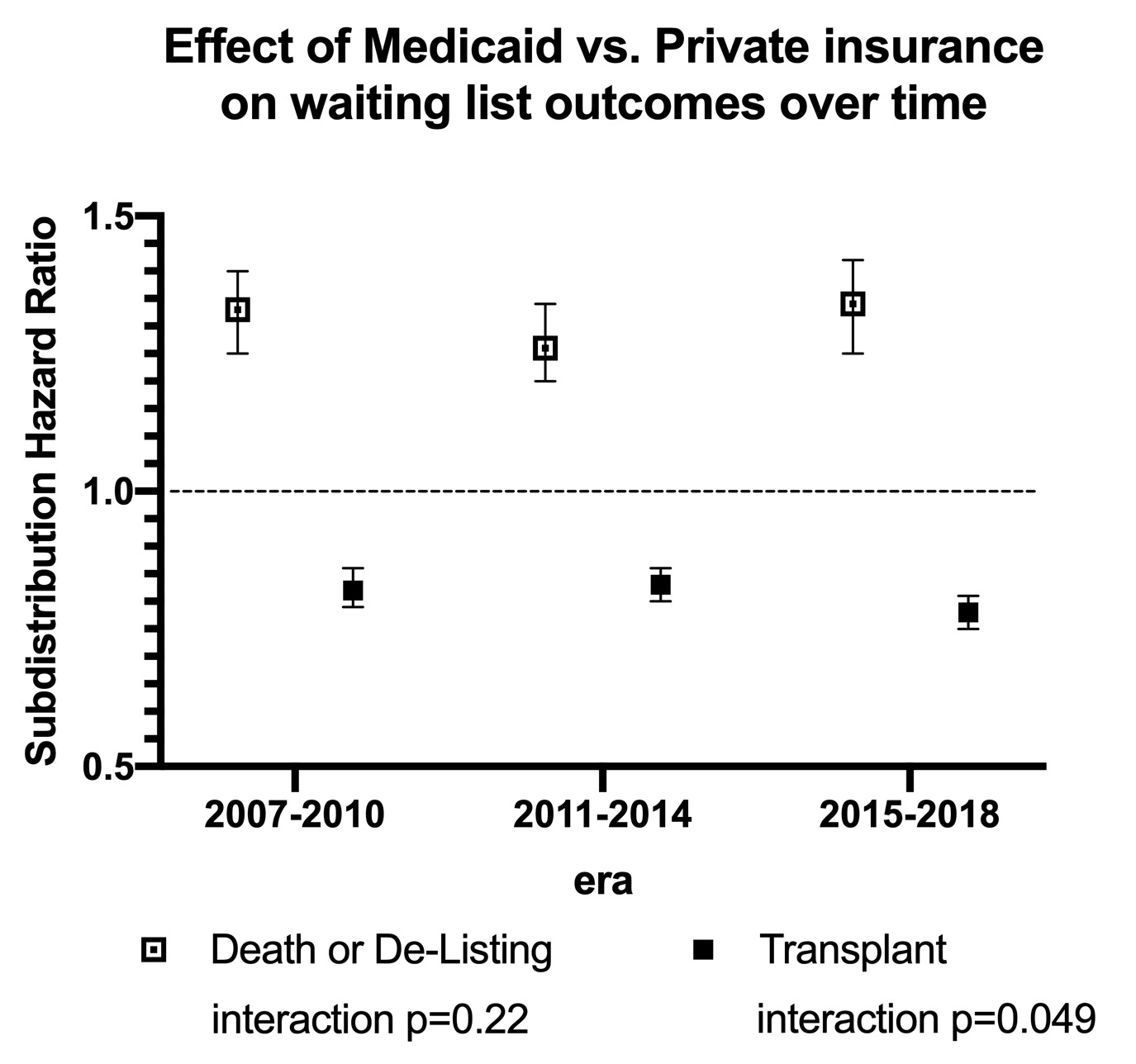
*Methods: We conducted a retrospective cohort study of liver transplant candidates and assessed changes in payor sources and outcomes in the years before (2007-2010), during (2011-2014), and after (2015-2018) ACA implementation. For waitlist outcomes (death/delisting and transplant), multivariable competing risks models were used to estimate sub-distribution hazard ratios (SHR), with interaction terms used to assess the changing impact of insurance over time. Poisson models were used to estimate incidence rate ratios (IRR) for inactivations within the first year. For transplant outcomes, Cox proportional hazards models were used to estimate the effect of insurance status on death and graft loss over time.
*Results: In our cohort of 121,298 liver waitlisted candidates, the proportion insured by Medicaid increased over time (Table 1). Medicaid patients had higher risk of death or de-listing (SHR 1.31 95%CI 1.26-1.35, p<0.001) and lower risk of receiving transplant (SHR 0.81 95%CI 0.79-0.83, p<0.001) than those privately-insured. After 2014, the likelihood of transplant for Medicaid candidates further decreased (Figure 1). Medicaid-insured patients had a higher rate of inactivation within the first year on the waiting list than the privately insured (IRR 1.20 95%CI 1.19-1.20,p<0.001). Among those receiving liver transplant, Medicaid-insured patients had higher risk of death (HR 1.16 95% CI 1.11-1.21,p<0.001) and graft loss (HR 1.20 95%CI 1.14-1.25, p<0.001); these risks did not significantly change over time.
*Conclusions: Medicaid expansion via the ACA is associated with an increase in the number of patients listed for liver transplant, but these patients continue to have inferior waitlist and post-transplant outcomes relative to the privately insured.
| Characteristic | 2007-2010.(n=38,575) | 2011-2014.(n=39,656) | 2015-2018. (n=43,067) | p-value |
| Initial Expansion | n=20,364 | n=20,803 | n=22,234 | |
| Medicaid | 3,625 (17.8%) | 4,059 (19.5%) | 5,225 (23.5%) | <0.001 |
| Later Expansion | n=5,024 | n=4,774 | n=5,025 | |
| Medicaid | 739 (14.5%) | 758 (15.9%) | 885 (17.6%) | <0.001 |
| No Expansion | n=12,996 | n=13,843 | n=15,639 | |
| Medicaid | 1,559 (12.0%) | 1,751 (12.6%) | 1,598 (10.2%) | <0.001 |
Figure 1. Effect of Medicaid vs Private insurance on liver transplant waitlist outcomes, by era.
To cite this abstract in AMA style:
Shaw BI, Samoylova ML, Wang V, Jr TRisoli, Peskoe S, Caddell K, McElroy LM. The Effect of the Affordable Care Act on Insurance Status, Waitlist, and Transplant Outcomes in Liver Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/the-effect-of-the-affordable-care-act-on-insurance-status-waitlist-and-transplant-outcomes-in-liver-transplantation/. Accessed February 28, 2026.« Back to 2021 American Transplant Congress