Stanford Integrated Psychosocial Assessment for Transplant Predicts Immunosuppression Non-Adherence after Liver Transplantation
S. Deutsch-Link1, E. Weinberg2, M. McDougal3, L. Jones4, T. Bitterman2, M. Serper2
1Medicine, University of Pennsylvania, Philadelphia, PA, 2Gastroenterology & Hepatology, University of Pennsylvania, Philadelphia, PA, 3Drexel University, Philadelphia, PA, 4PCOM, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: B-134
Keywords: Immunosuppression, Psychosocial, Rejection
Session Information
Session Name: Poster Session B: Liver: Immunosuppression and Rejection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Patients with end-stage liver disease presenting for liver transplant (LT) evaluation have a high burden of psychosocial comorbidities. The Stanford Integrated Psychosocial Assessment for Transplant (SIPAT) is one of the most commonly used psychosocial assessments in LT evaluation, however, its impact on post-LT outcomes is not well-known. Our aims were to assess the relationship between SIPAT score and 1) immunosuppression non-adherence, 2) allograft rejection, and 3) mortality.
*Methods: We conducted a retrospective cohort study of 287 LT recipients from 2014-2018. Patients were divided into two groups: “Good Candidate” (SIPAT<21) vs “Minimally Acceptable Candidate” (SIPAT>21), according to the validated SIPAT scoring system. Tacrolimus level variability was measured by the tacrolimus coefficient of variation (CoV), a validated non-adherence assessment shown to predict rejection. Tacrolimus levels and allograft rejection within 3 months of LT were excluded. Multivariable regression assessed the impact of SIPAT score on tacrolimus CoV. Multivariable cox proportion hazard models assessed the relationship between SIPAT scores and allograft rejection and mortality.
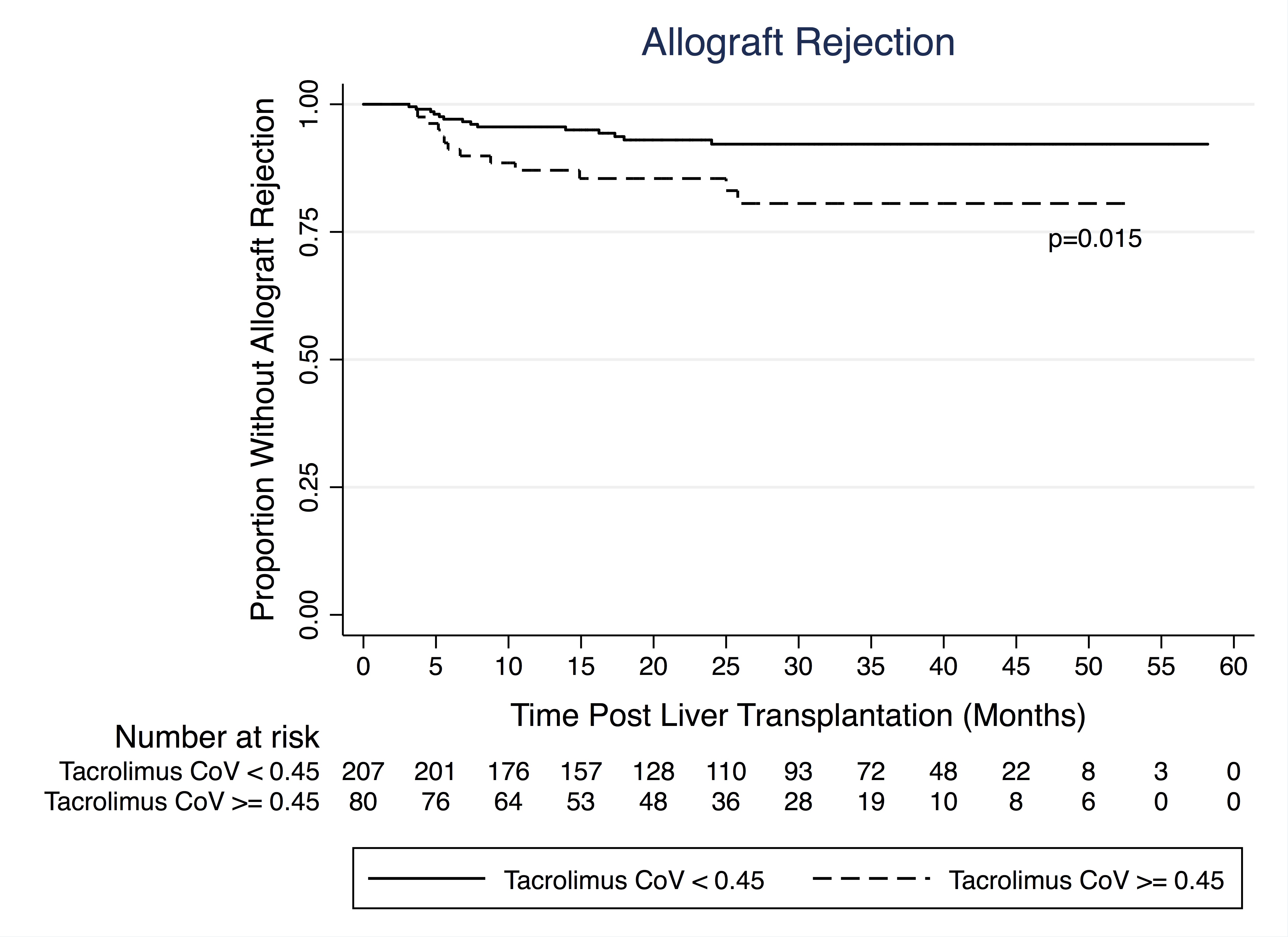
*Results: In a multivariable model adjusted for age, gender, race, MELD-Na, and liver disease etiology, SIPAT >21 was significantly associated with a tacrolimus CoV >0.45 (OR 2.47, CI 1.34-4.54; p=0.004). (Table 1) Adjusted time-to-event analyses demonstrated no significant relationship between SIPAT and allograft rejection or patient mortality (p=0.65 and p=0.95, respectively). Tacrolimus CoV >0.45 predicted allograft rejection (HR 2.52, CI 1.11-5.7, p=0.015). (Figure 1)
*Conclusions: Higher SIPAT scores, which represent higher psychosocial risk, were associated with higher tacrolimus level variability, but not associated with allograft rejection or patient mortality, possibly due to sample size. Future studies assessing long-term outcomes are needed to better understand the predictive role of SIPAT.
| Variable | OR | 95% CI | P-Value |
| SIPAT >= 21 | 2.47 | 1.34-4.54 | 0.004* |
| Age at Transplant | 0.98 | 0.96-1.01 | 0.147 |
| Gender | 1.37 | 0.75-2.49 | 0.307 |
| MELD-Na | 0.88 | 0.60-1.29 | 0.511 |
| Race | 0.98 | 0.96-1.01 | 0.162 |
| Liver Disease Etiology | 0.96 | 0.83-1.11 | 0.560 |
To cite this abstract in AMA style:
Deutsch-Link S, Weinberg E, McDougal M, Jones L, Bitterman T, Serper M. Stanford Integrated Psychosocial Assessment for Transplant Predicts Immunosuppression Non-Adherence after Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/stanford-integrated-psychosocial-assessment-for-transplant-predicts-immunosuppression-non-adherence-after-liver-transplantation/. Accessed March 1, 2026.« Back to 2020 American Transplant Congress