Simultaneous Robot-Assisted Bilateral Native Nephrectomy and Kidney Transplantation for Polycystic Kidney Disease
University of Maryland, Baltimore, Baltimore, MD
Meeting: 2022 American Transplant Congress
Abstract number: 1389
Keywords: Kidney, Kidney transplantation, Laparoscopy, Polycystic kidney disease
Topic: Clinical Science » Kidney » 41 - Kidney Technical
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Simultaneous bilateral native nephrectomy (NNx) and kidney transplantation is the preferred treatment for patients with end-stage renal disease (ESRD) due to symptomatic polycystic kidney disease (PKD). However, the morbidity of simultaneous surgery can be high in overweight and obese patients, particularly in regard to wound complications. To improve outcomes and offer simultaneous NNx and transplant to larger patients, we now offer a fully robotic-assisted approach. We present our early experience and technique.
*Methods: We present the case of 52 yo male with BMI of 33 affected by end-stage renal disease (ESRD) due to PKD (creatinine: 8.86 mg/dL; GFR: 8 ml/min per 1.73 m(2)) who received a preemptive living-donor kidney. Pre-operatively he suffered from severe abdominal distension and early satiety.
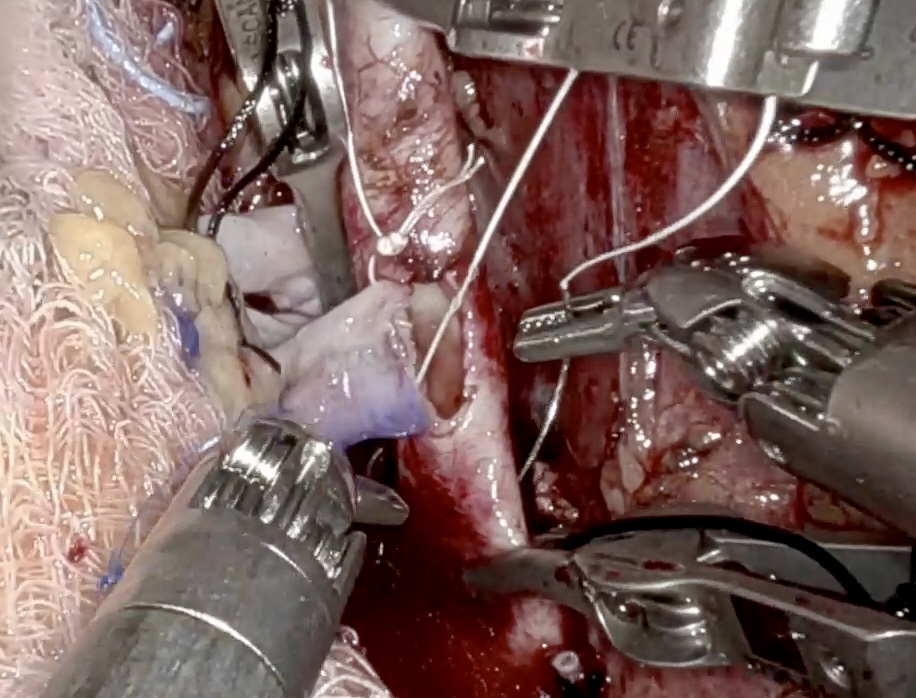
*Results: The robotic-assisted bilateral nephrectomy was started and the donor case was then initiated once both native kidneys were fully mobilized with hila controlled. The recipient team then proceeded with extraction of both kidneys througha 7-cm periumbilical incision. Once both kidneys were out, the recipient was re-positioned from flank to Trendelenburg, steroids and Alemtuzumab induction were given, and a robotic-assisted kidney transplant (RKT) was performed in the right iliac fossa. The kidney was replaced in the retroperitoneum in standard position at the conclusion of the case. The surgical time was 403, 174min for the donor nephrectomy, and 206 minutes for the RKT with 41 minutes of anastomosis time. The estimated blood loss was 50 ml in the donor and 300 ml in the recipient. Cold ischemia time was 2.6h. The kidney started to produce urine intra-operatively with a rate of >500 cc/h and a routine post-transplant ultrasound showed patent vessels with no immediate complication. The patient started ambulating and taking oral intake by postoperative day 1. He received a PCA per our standard protocol but did not use any oral narcotics once he was tolerating PO intake. There were no postoperative complications, and the patient was discharged from the hospital on postoperative day 4 with a creatinine of 1.57 mg/dL.
*Conclusions: We present a transperitoneal simultaneous robot-assisted bilateral native nephrectomy and pre-emptive kidney transplantation. This approach has the potential to decrease incision-related complications of simultaneous open surgery while preserving his pre-emptive status, reducing hospital stay, and offering enhanced visualization for vascular anastomosis.
To cite this abstract in AMA style:
Meier R, Carrier A, Crane A, Alvarez-Casas J, Maluf D, Bhati C. Simultaneous Robot-Assisted Bilateral Native Nephrectomy and Kidney Transplantation for Polycystic Kidney Disease [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/simultaneous-robot-assisted-bilateral-native-nephrectomy-and-kidney-transplantation-for-polycystic-kidney-disease/. Accessed March 9, 2026.« Back to 2022 American Transplant Congress