Sex- and Insurance- Based Disparities in Listing for and Benefit from Simultaneous Heart-Kidney Transplant
1Stanford University School of Medicine, Stanford, CA, 2Duke University School of Medicine, Durham, NC
Meeting: 2022 American Transplant Congress
Abstract number: 1202
Keywords: Heart transplant patients, Kidney transplantation, Medicare, Organ Selection/Allocation
Topic: Clinical Science » Organ Inclusive » 70 - Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Information
Session Name: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Rates of simultaneous heart-kidney (SHK) transplant vary widely in the United States (US). Absent uniform eligibility criteria, sex and insurance status could influence patient selection, with subsequent disparities in transplant access and outcomes.
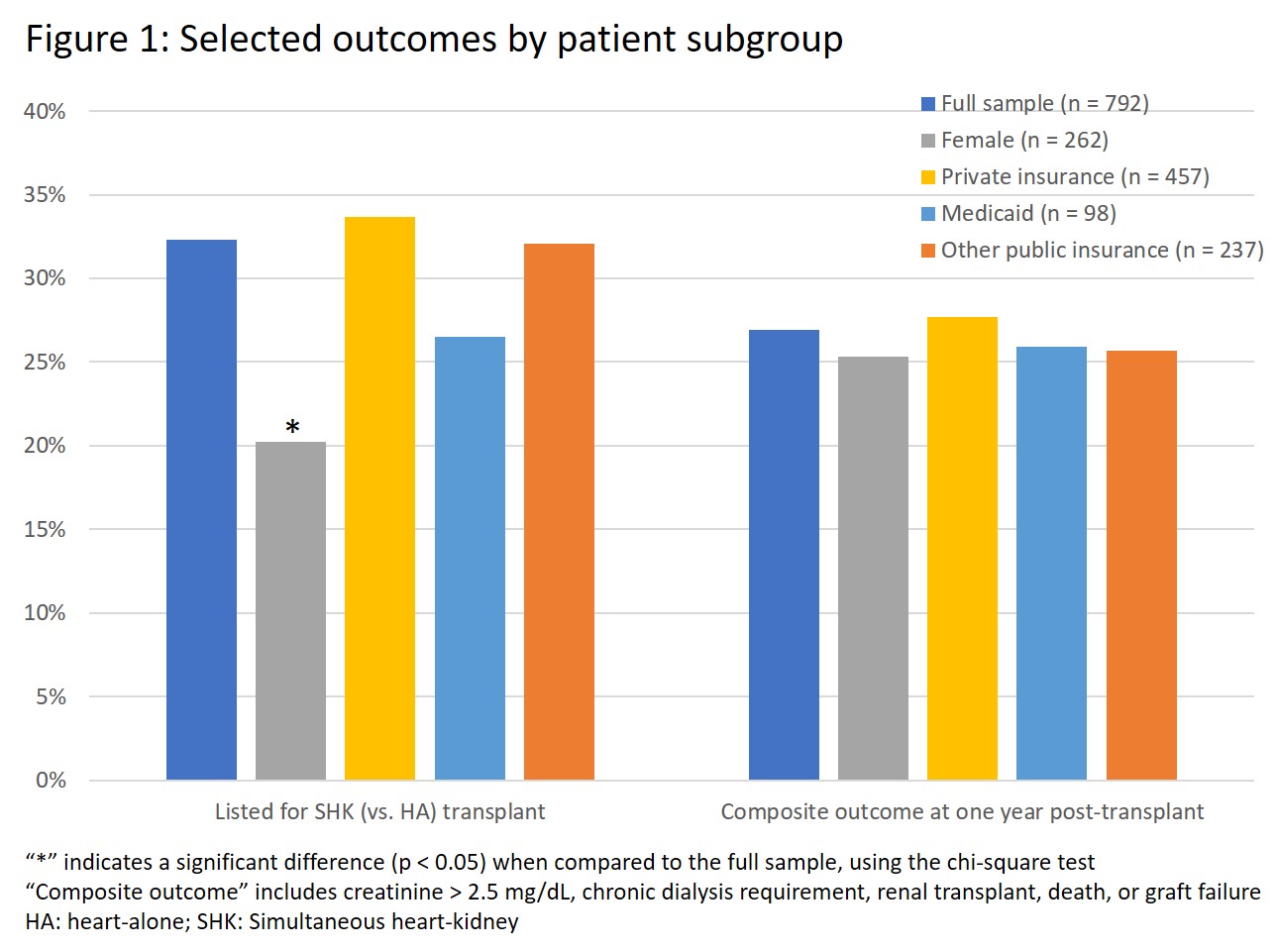
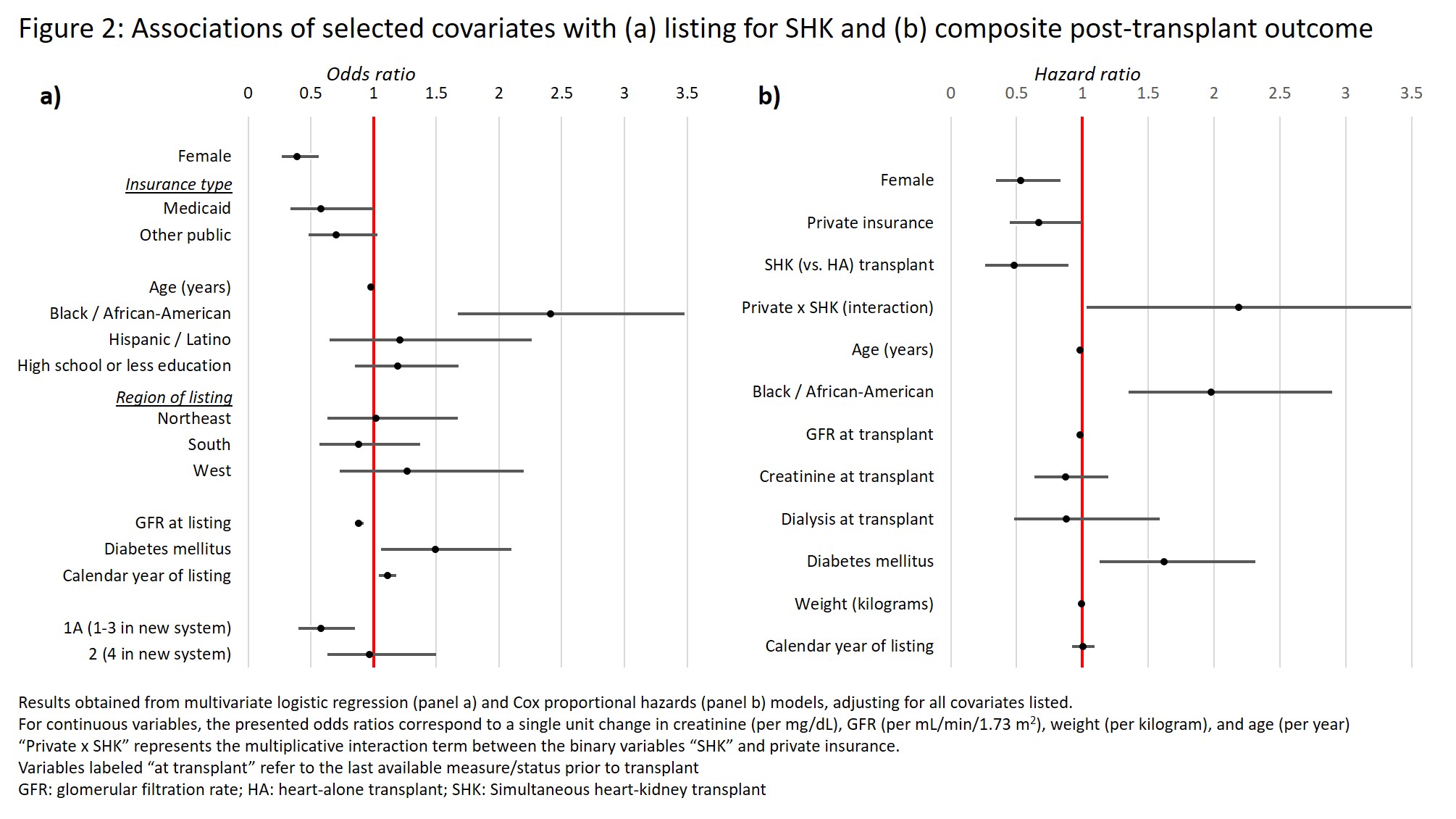
*Methods: We included adults (age 18-60 years) listed for heart-alone (HA) or SHK transplant in the US in 2010-2018, who were not on dialysis at listing and had glomerular filtration rate of 20-35 mL/min/1.73 m2. We assessed differences in rates of SHK listing and post-transplant outcomes by sex and primary insurance type, before and after adjustment for demographic and clinical risk factors. The primary outcome was a composite of death, graft failure, creatinine > 2.5 mg/dL, dialysis dependence, and kidney transplant in the first year after transplant.
*Results: Of 792 patients included, 33% were female, 32% were SHK-listed, and 58%, 12%, and 30% had private, Medicaid, and other public insurance, respectively. Females were less likely to be SHK-listed (adjusted OR = 0.39, p < 0.001) and had lower risk of the primary outcome (adjusted HR = 0.53, p = 0.006). Medicaid (vs. privately insured) patients were also less likely to be SHK-listed (adjusted OR = 0.58, p = 0.048). Among those receiving HA transplant, unadjusted risk of the primary outcome differed significantly by insurance type (p = 0.027 by log-rank test) and was highest among those with public insurance; there was no such disparity among those receiving SHK. In multivariate analysis, publicly (vs. privately) insured patients had higher adjusted risk of the primary outcome (HR = 1.49, p = 0.049). There was a significant interaction between insurance type and receipt of SHK transplant (p = 0.042), such that SHK conferred a significant risk reduction (HR = 0.48, p = 0.020) for those with public (but not private) insurance.
*Conclusions: Among candidates for SHK transplant, those with public (vs. private) insurance were less likely to be listed for SHK – despite a greater apparent benefit from it – and had worse post-transplant outcomes . These disparities are not explained by measured clinical factors and may stem from differential access to or quality of care.
To cite this abstract in AMA style:
Wayda B, Cheng XS, Garcia P, Sanoff S, McElroy LM, Khush KK. Sex- and Insurance- Based Disparities in Listing for and Benefit from Simultaneous Heart-Kidney Transplant [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/sex-and-insurance-based-disparities-in-listing-for-and-benefit-from-simultaneous-heart-kidney-transplant/. Accessed March 5, 2026.« Back to 2022 American Transplant Congress