Rural Dialysis Facilities are Associated with Better Dialysis Quality but Less Home Dialysis Use
1Surgery, Brigham and Women's Hospital, Boston, MA, 2Medicine, Boston Medical Center, Boston, MA
Meeting: 2021 American Transplant Congress
Abstract number: 288
Keywords: Waiting lists
Topic: Clinical Science » Organ Inclusive » Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Information
Session Name: Disparities in Access and Outcomes in Kidney Transplantation
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 7, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:35pm-6:40pm
Presentation Time: 6:35pm-6:40pm
Location: Virtual
*Purpose: Dialysis facility quality is associated with patient outcomes. The 60 million rural dwellers across the United States are older, more likely to live in poverty, and more likely to be either underinsured or uninsured compared to their urban counterparts. 240,000 of these rural dwellers have ESKD; it is unknown if differences in dialysis facility size and quality exist between urban and rural settings.
*Methods: Using the 2017 United States Renal Data System Facility File and Medicare Dialysis Facility Compare, we identified 1,472 (19.7%) rural and 6,008 (80.3%) urban dialysis facilities as classified by Rural Urban Commuting Area codes. Differences in characteristics, resources, and patient outcomes were assessed between rural and urban facilities.
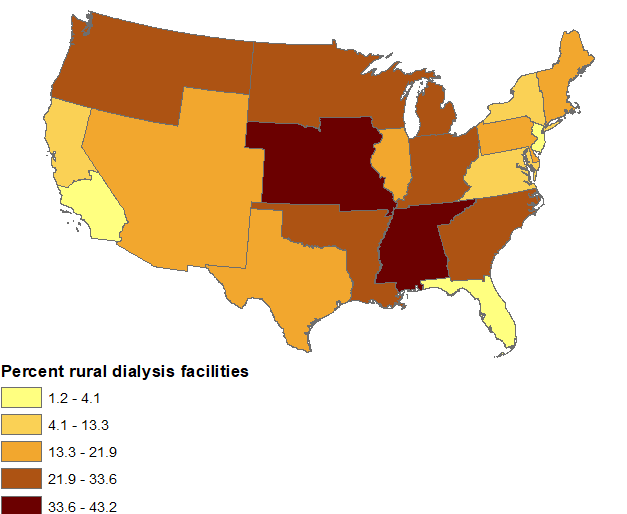
*Results: There was significant variability in the proportion of rural dialysis facilities across the ESRD Networks (Figure, P<0.001). Rural dialysis facilities were more likely to be non-profit (19.7 vs. 11.9%, P<0.001). Rural facilities were smaller (median dialysis stations 13 vs. 18, P<0.001), but had more support staff: fewer patients per social worker (41 vs 65, P<0.001) and patients per nurse (12 vs. 15, P<0.001). Rural facilities had fewer patients on home dialysis (median 7.4 vs 13.7%, P<0.001). In terms of quality metrics, there was no association with mean standardized mortality (1.01 vs. 1.02, P=0.08) or transfusion ratios (1.02 vs. 1.00, P=0.18), but the mean standardized hospitalization ratio (0.86 vs. 1.04, P<0.001) and 90-day catheter infection rates (10.2 vs. 10.6%, P=0.01) were lower for rural facilities.
*Conclusions: Facility size and quality metrics vary among rural and urban dialysis facilities. Rural facilities had more staffing resources and better ESKD quality metrics, but surprisingly had fewer patients on home dialysis. Further work is needed to assess impact of dialysis facility quality on long-term rural ESKD outcomes, as well as to improve the number of patients on home dialysis.
To cite this abstract in AMA style:
Adler JT, Xiang L, Waikar SS. Rural Dialysis Facilities are Associated with Better Dialysis Quality but Less Home Dialysis Use [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/rural-dialysis-facilities-are-associated-with-better-dialysis-quality-but-less-home-dialysis-use/. Accessed March 6, 2026.« Back to 2021 American Transplant Congress