Risk of Clostridioides Difficile Infection After Kidney Transplant
C. Thomas1, B. Crowther2, K. Schwarz2, D. Chen1, Y. Shandaliy1, K. Johnson1, P. Klem2
1Skaggs School of Pharmacy and Pharmaceutical Sciences, University of Colorado, Anschutz Medical Campus, Aurora, CO, 2Skaggs School of Pharmacy and Pharmaceutical Sciences, University of Colorado Hospital System, Aurora, CO
Meeting: 2022 American Transplant Congress
Abstract number: 970
Keywords: Bacterial infection, High-risk, Reinfection, Risk factors
Topic: Clinical Science » Infection Disease » 24 - All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: All Infections (Excluding Kidney & Viral Hepatitis) II
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: For patients undergoing kidney transplant, the risk of developing Clostridioides difficle infection (CDI) is reported to be 4.7%, likely due to risk factors such as immunosuppression, concurrent antibiotic use, and hospitalization. When looking at patients in the general population with a history of CDI, there is a reported 20 – 30% increased risk of experiencing reinfection, suggesting that a prior history of CDI could be another risk factor for transplant recipients. The purpose of this study is to identify risk factors associated with CDI within 90 days after kidney transplant.
*Methods: A retrospective cohort study was conducted to compare risk of CDI in kidney transplant recipients with a pre-transplant history of CDI to a historical control population without a history of CDI in patients transplanted between 2011-2021. Inclusion criteria were age > 18 years, history of kidney transplant, and clinical diagnosis of CDI in the pre-transplant CDI group. The primary outcome was incidence of CDI 90 days post-transplant. The secondary outcome was incidence of CDI within one-year post-transplant. Subgroup analyses included race, delayed graft function (DGF), proton-pump inhibitor use, and mean length of index hospital stay.
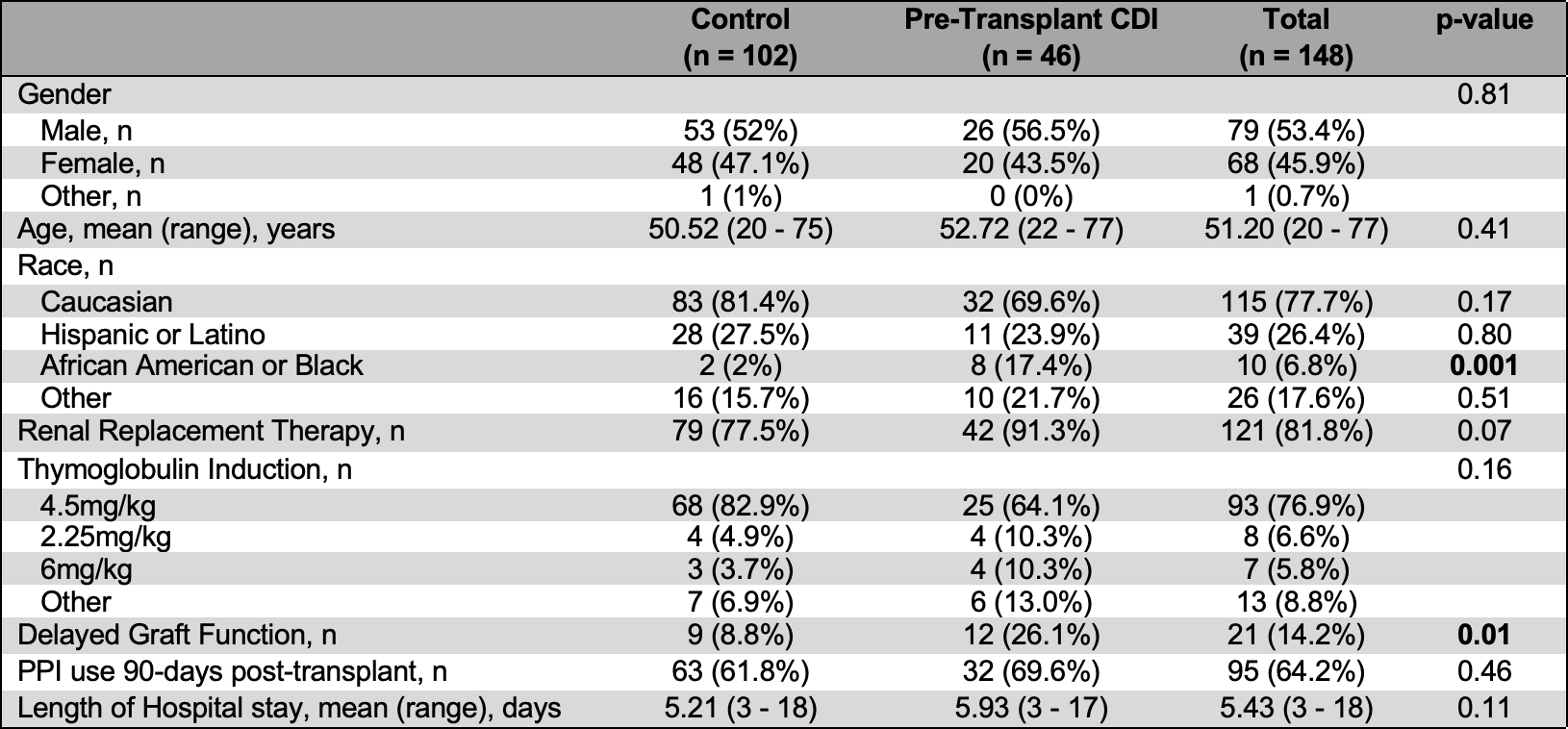
*Results: 148 kidney transplant recipients within the UCHealth system were included (46 pre-transplant CDI, 102 control). See table 1 for baseline characteristics, which were not significant between groups besides incidence of DGF. The mean (SD) time to CDI was 530 ± 557 days pre-transplant vs 341 ± 575 days control. Incidence of CDI 90 days post-transplant was 15.2% pre-transplant CDI vs 2.9% control (p = 0.01). Incidence of CDI one-year post-transplant was 28.3% pre-transplant vs 5.9% control (p < 0.001). 26.1% subjects in the pre-transplant CDI population experienced DGF vs 8.8% in the control group (p = 0.01).
*Conclusions: Kidney transplant recipients with a history of CDI prior to transplant have a significantly increased risk of CDI 90 days and 365 days after transplant. This important risk factor highlights the need to evaluate CDI prophylaxis, with oral vancomycin or fidaxomicin, in this population. Further investigation regarding the association between pre-transplant CDI and delayed graft function is warranted.
To cite this abstract in AMA style:
Thomas C, Crowther B, Schwarz K, Chen D, Shandaliy Y, Johnson K, Klem P. Risk of Clostridioides Difficile Infection After Kidney Transplant [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/risk-of-clostridioides-difficile-infection-after-kidney-transplant/. Accessed February 23, 2026.« Back to 2022 American Transplant Congress