Retroperitoneoscopic Native Nephrectomy in Renal Transplant Recipients with Autosomal Dominant Polycystic Kidney Disease
1Hokkaido University Hospital, Sapporo, Japan, 2Urology, Hokkaido University Hospital, Sapporo, Japan, 3Urology, Kushiro City General Hospital, Kushiro, Japan, 4Urology, Asahikawa City General Hospital, Asahikawa, Japan
Meeting: 2019 American Transplant Congress
Abstract number: C146
Keywords: Kidney transplantation, Laparoscopy, Nephrectomy, Polycystic kidney disease
Session Information
Session Name: Poster Session C: Kidney Technical
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Autosomal dominant polycystic kidney disease (ADPKD) leads to end stage kidney disease (ESKD) and the need for kidney transplantation (KTX). Native nephrectomy is required when the polycystic kidneys are too large to safely implant a kidney in the iliac fossa. Open nephrectomy (ON) using a flank incision for KTX is extremely invasive. Although transperitoneal laparoscopic nephrectomy for kidneys affected by ADPKD has been reported by some centers, the retroperitoneal approach ispreferred, because the kidney is implanted in retroperitoneal space. Therefore, we used retroperitoneoscopic native nephrectomy (RN) for ADPKD.
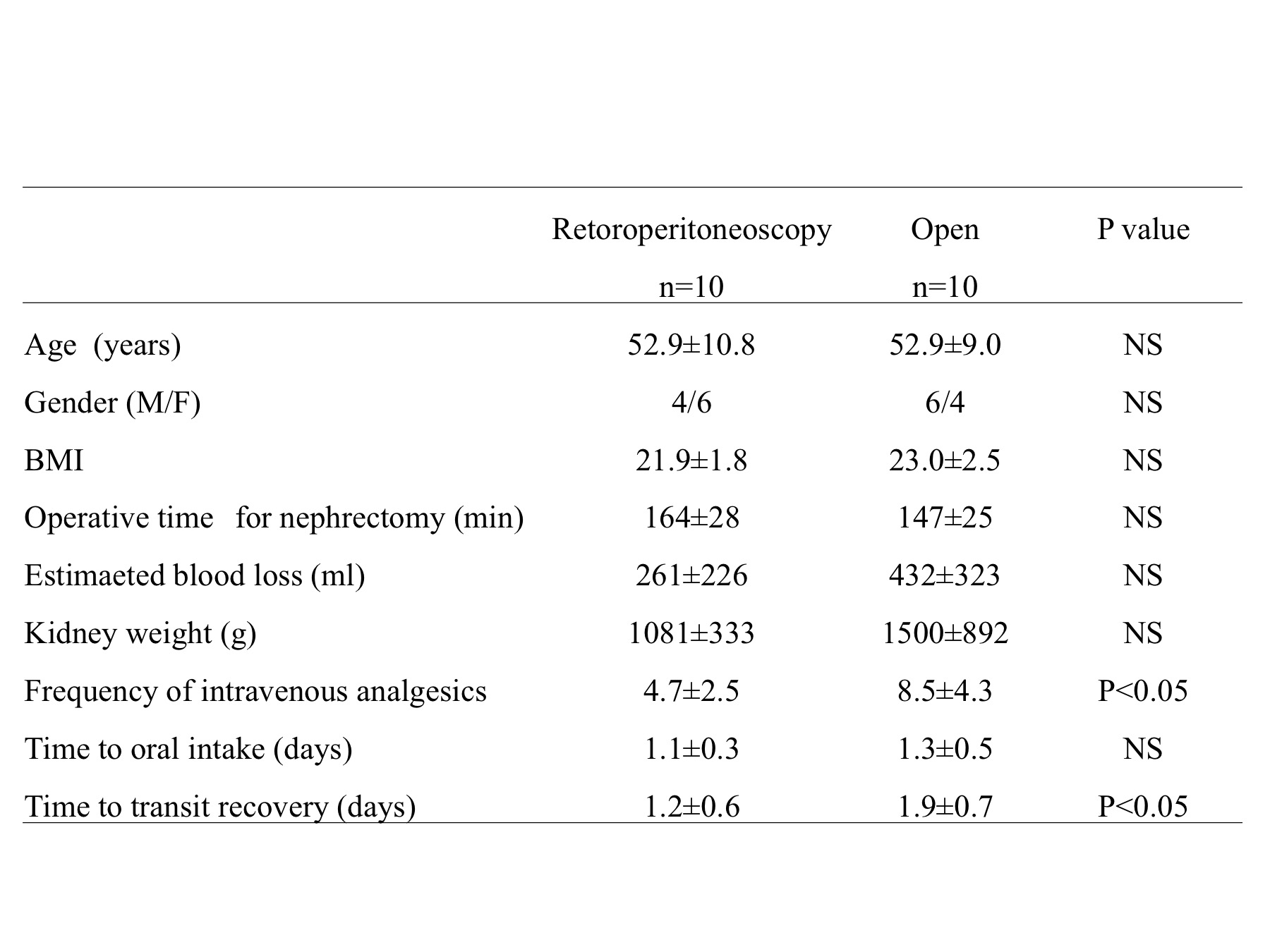
*Methods: Twenty consecutive kidney recipients (10 men, 10 women) were enrolled in this study. The mean age of the recipients was 54.5 ± 9.6 years. Unilateral native nephrectomy was performed to allow for the creation of sufficient space just before KTX. RN was performed for 10 recipients, and ON for 10 recipients. In the RN procedure, the kidney is completely delivered with 4 ports (12mm×2 ports and 5mm×2 ports) and the kidney is then extracted through Gibson incision (15cm) made for KTX. In ON, the flank incision (20cm) for nephrectomy was made, followed by the Gibson incision (15cm) for KTX. We compared the perioperative outcomes and early complications for the two procedures.
*Results: There was no difference in the age, gender and body mass index of the patients between the two groups. The operative time for nephrectomy, intraoperative blood loss and nephrectomized kidney weight were similar between the two groups. Conversion to open surgery was not observed in RN group. Although there was no intraoperative complication observed in RN, a pleura injury led to the insertion of thoracostomy catheter in the ON group. The frequency of post-operative analgesics was significantly lower in RN group compared to that in ON group (4.7 VS. 8.5 times, P<0.05). Furthermore, the time to transit recovery was significantly shorter in RN group than in ON group (1.2 vs. 1.9 days, P<0.05). There were no severe post-operative complications in both groups.
*Conclusions: RN for ADPKD in KTX is well-tolerated and is less invasive compared to open surgery. These results suggest that RN could be a feasible option for nephrectomy with ADPKD undergoing KTX.
To cite this abstract in AMA style:
Hotta K, Iwami D, Furumido J, Morita K, Tanabe T, Mochizuki T, Higuchi H, Iwahara N, Abe T, Kanagawa K, Shinohara N. Retroperitoneoscopic Native Nephrectomy in Renal Transplant Recipients with Autosomal Dominant Polycystic Kidney Disease [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/retroperitoneoscopic-native-nephrectomy-in-renal-transplant-recipients-with-autosomal-dominant-polycystic-kidney-disease/. Accessed March 5, 2026.« Back to 2019 American Transplant Congress