Reduced Conversion from IgM Anti-HLA-DSA to IgG Anti-HLA-DSA in Belatacept-Treated vs. Cyclosporine-Treated Patients in BENEFIT and BENEFIT-EXT Trials.
1Terasaki Foundation Laboratory, Los Angeles, CA
2Bristol-Myers Squibb, Lawrenceville, NJ
3Emory University, Atlanta, GA
Meeting: 2017 American Transplant Congress
Abstract number: 167
Keywords: Antibodies, Immunosuppression
Session Information
Session Name: Concurrent Session: Novel Immunosuppression - DSA Monitoring
Session Type: Concurrent Session
Date: Sunday, April 30, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:42pm-4:54pm
Presentation Time: 4:42pm-4:54pm
Location: E450b
Post-transplant, up to 50% of recipients develop IgM DSA. Half of these patients go on to develop IgG DSA. Importantly, patients that progress to IgG have significantly poorer outcomes than those who remain only IgM DSA positive. Thus, prevention of IgM to IgG isotype switching could be an ideal strategy to limit chronic rejection. In this study, we examined the DQB1* typed cohorts from the BENEFIT and BENEFIT-EXT studies and evaluated whether belatacept-treated patients have a lower rate of isotype switching.
Methods 374 patients were included in the analysis because they had HLA DQ (plus HLA A, B, and DR) typing information or were IgG DSA positive. IgM and IgG HLA antibody testing (single antigen beads) were conducted pre-transplant and 6, 12, 24, and 36 months post-transplant. IgG mean florescence intensity (MFI) over 2000 and IgM over 1000 were considered positive. Furthermore, IgG or IgM DSA appearing in the first month were considered “pre-formed” and those appearing after the first month post-transplant were considered de novo DSA (dnDSA).
Results 117 patients (31.3%) were IgM DSA (+) . The overall IgG DSA (+) rate was 29.7%. By treatment group, there was an equal distribution of patients developing IgM DSA (Table). Allograft survival in patients with only IgM DSA was significantly higher than in those patients who converted to IgG DSA (Figure, p=0.0008). Overall, the cyclosporine (CsA) group had a significantly higher proportion of IgG DSA (+) cases than the belatacept groups (p=0.002). Conversion from pre-formed IgM DSA to de novo IgG DSA in patients with pre-formed IgM DSA was similar between belatacept-LI and CsA groups but substantially lower for the belatacept-MI group. Among those with IgM dnDSA, the conversion to IgG dnDSA was highest in the CsA group compared to the belatacept groups (p=0.04).
Conclusion IgM DSA does not impact long term allograft survival. Therefore, belatacept's ability to prevent conversion of IgM (+) DSA to IgG (+) dnDSA may provide a major therapeutic benefit.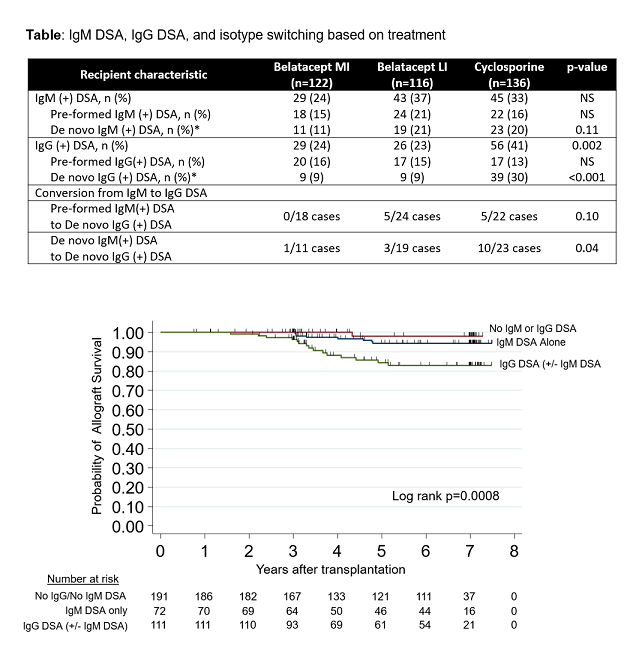
CITATION INFORMATION: Everly M, Townsend R, Gebel H, Bray R. Reduced Conversion from IgM Anti-HLA-DSA to IgG Anti-HLA-DSA in Belatacept-Treated vs. Cyclosporine-Treated Patients in BENEFIT and BENEFIT-EXT Trials. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Everly M, Townsend R, Gebel H, Bray R. Reduced Conversion from IgM Anti-HLA-DSA to IgG Anti-HLA-DSA in Belatacept-Treated vs. Cyclosporine-Treated Patients in BENEFIT and BENEFIT-EXT Trials. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/reduced-conversion-from-igm-anti-hla-dsa-to-igg-anti-hla-dsa-in-belatacept-treated-vs-cyclosporine-treated-patients-in-benefit-and-benefit-ext-trials/. Accessed February 18, 2026.« Back to 2017 American Transplant Congress
