Recipient and Kidney Allograft Outcomes from Hypertensive Live-Donor in the United States
1Medicine, University of Minnesota, Minneapolis, MN, 2Complex Care Analytics, M-Health Fairview, Minneapolis, MN, 3School of Public Health, University of Minnesota, Minneapolis, MN, 4Surgery, University of Minnesota, Minneapolis, MN
Meeting: 2021 American Transplant Congress
Abstract number: 470
Keywords: Donation, Hypertension, Kidney transplantation, Outcome
Topic: Clinical Science » Kidney » Kidney Living Donor: Selection
Session Information
Session Time: 7:30pm-8:30pm
 Presentation Time: 7:40pm-7:50pm
Presentation Time: 7:40pm-7:50pm
Location: Virtual
*Purpose: Controlled hypertension in select prospective kidney donors is no longer an exclusion criterion for donation. We examined the association between pre-donation hypertension (HTN) and both mortality and death censored kidney graft survival in recipients.
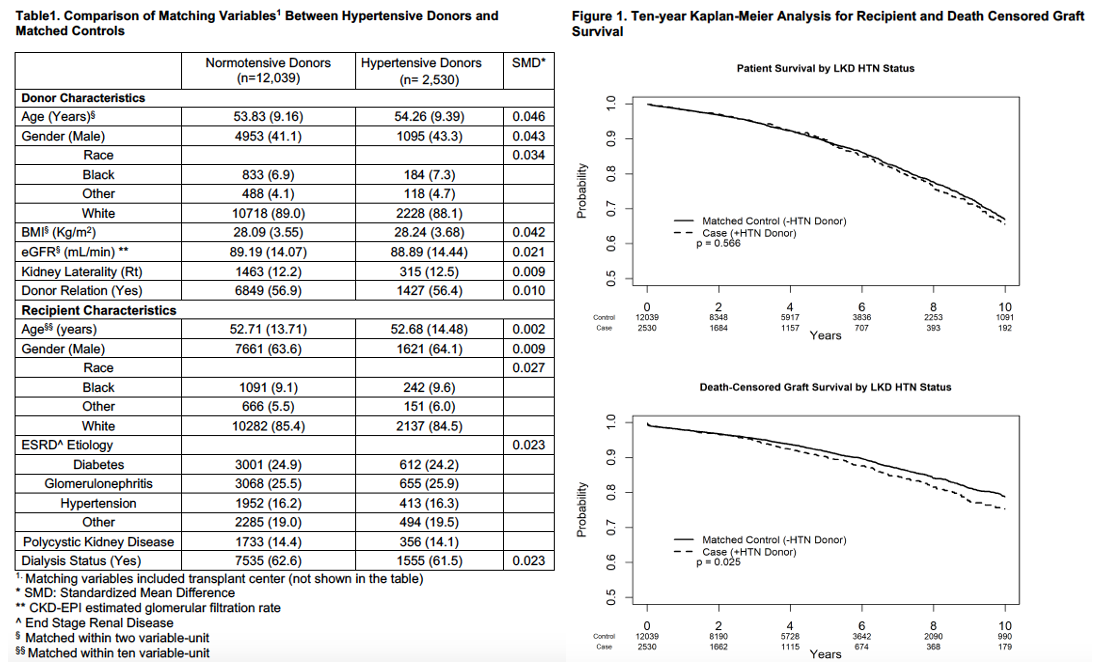
*Methods: Between 2004 and 2019, we identified 2574 donors with HTN in the SRTR who had complete data for matching. Hypertensive donors were matched at 1:5 to normotensive donors, within the same transplant center, based on donor and recipient characteristics. Propensity matching was used to balance the cases and controls. All matching variables were evenly balanced between groups with SMD <0.05 (Table 1). 44 donors were not matched. Unweighted Kaplan-Meier curves were generated through 10 years from engraftment for the recipient survival (RS) and death-censored graft survival (DCGS) by donor hypertension status. Weighted Cox proportional hazard models (with each case-control group as a random effect) were used to examine the association between donor-HTN and outcomes of interest. In addition to the matching variables, models were adjusted for induction type, XM-status, HLA-MM, and immunosuppression maintenance. The RS model was stratified by transplant year, and the DCGS model was stratified by transplant year and immunosuppression maintenance due to non-proportional hazards.
*Results: Hypertensive live-donor kidney utilization increased over time. DGF rate did not differ between groups. At 1-year from engraftment, eGFR was 2.3 mL/min lower (p=0.003), and the rejection rate was 1.5% higher (p=0.038) in the recipients of hypertensive donor kidneys. In the unweighted Kaplan-Meier analysis (Figure 1), RS did not differ by donor-HTN status (log-rank p=0.566). DCGS was slightly lower in recipients of hypertensive donor kidneys (log-rank p=0.025). In the multivariable weighted Cox PH models, compared to normotensive donors, kidneys from hypertensive donors were not associated with worse RS (95%LLCI, aHR, 95%ULCI) (0.93,1.06,1.21), or DCGS (0.99, 1.16,1.36).
*Conclusions: In this large propensity-matched cohort of live kidney donors and their recipients, donor hypertension was not associated with inferior recipient or graft survival after multivariable adjustment. The judicious utilization of kidneys from hypertensive donors in the United States appears safe for recipients. Expanding the donor pool with select hypertensive donors is a viable option.
To cite this abstract in AMA style:
Riad S, Jackson S, Vock D, Matas A. Recipient and Kidney Allograft Outcomes from Hypertensive Live-Donor in the United States [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/recipient-and-kidney-allograft-outcomes-from-hypertensive-live-donor-in-the-united-states/. Accessed February 17, 2026.« Back to 2021 American Transplant Congress