Racial Barriers to Kidney Transplant After Listing, 2015 – 2020
1Nephrology, Hennepin Healthcare Research Institute, Minneapolis, MN, 2Scientific Registry of Transplant Recipients, Minneapolis, MN, 3Nephrology, Hennepin Healthcare, Minneapolis, MN
Meeting: 2022 American Transplant Congress
Abstract number: 513
Keywords: African-American, Allocation, Kidney transplantation
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Name: Health Equity and Access II
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:20pm-6:30pm
Presentation Time: 6:20pm-6:30pm
Location: Hynes Ballroom C
*Purpose: We sought to evaluate racial disparities in access to deceased donor kidney transplant (DDKT) following changes to kidney allocation system (KAS) implemented in 2014. We also aimed to identify candidate factors that were responsible for reducing African American (AA) access to transplant.
*Methods: This study used Scientific Registry of Transplant Recipient Data, and included all adult candidates for DDKT on the waitlist between Jan. 1, 2015 and Mar. 12, 2020 (n=233,033). Candidates were classified as African American (AA) or non-African American (non-AA) and categorical differences in waitlist activity and clinical factors were evaluated by chi-square tests. Univariable (e.g. AA race only) and multivariable (e.g. race and combinations of clinical factors) Cox models with the outcome of time to transplant were constructed to evaluate the impact of AA race on access to transplant. Sub-analysis were performed to account for potential confounding from inactive time and the COVID-19 era.
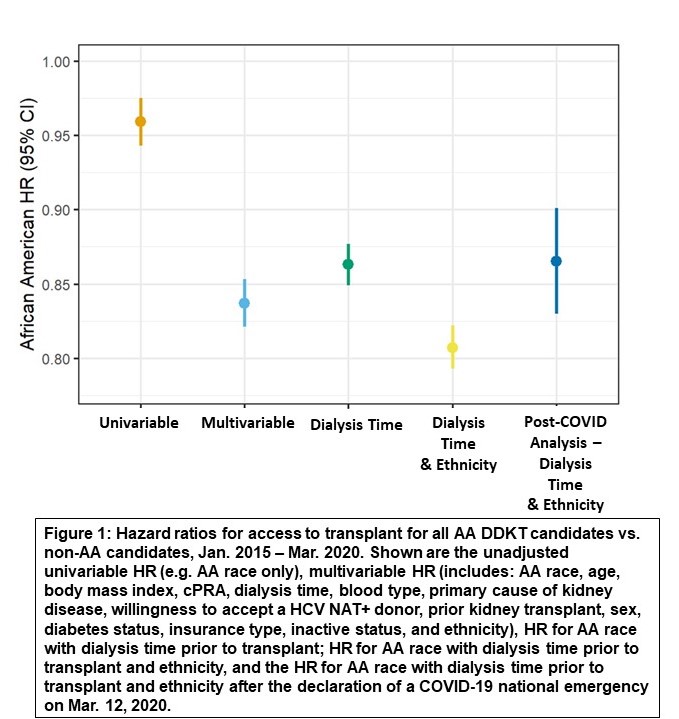
*Results: Of the 233,033 waitlisted candidates during the study period, 76,576 (32.9%) were AA. There were differences in the clinical profiles of AA and non-AA candidates. For instance, AA were more likely to have the following characteristics: higher BMI, blood type B, female, and have higher cPRA (all with p < 0.0001). AA had longer wait times and slower access to the waitlist after initiating dialysis (p < 0.0001). Our most complete multivariable model showed that AA were 16.3% less likely to receive DDKT, [HR: 0.837, (95% CI: 0.821, 0.852)] (Figure 1). Adjusting for dialysis time prior to listing [HR: 0.863 (95% CI: 0.849, 0.877)] and the combination of dialysis time prior to listing and ethnicity [HR: 0.807 (95% CI: 0.793, 0.822)] resulted in the biggest change in HR from the unadjusted model.
*Conclusions: AA have reduced access to DDKT when compared to non-AA in adjusted analyses. Dialysis time prior to listing and ethnicity are the biggest contributors to the disparity in access. The KAS provides increased access for patients with longer time on the waiting list, therefore, the unadjusted model has closer parity between AA and non-AA. However, even the unadjusted model still shows some disparity meaning that changes may still be necessary in the system by with DDK are allocated to candidates.
To cite this abstract in AMA style:
McKinney WT, Schladt D, Miller J, Weaver T, Pyke J, Madhusoodanan T, Israni AK. Racial Barriers to Kidney Transplant After Listing, 2015 – 2020 [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/racial-barriers-to-kidney-transplant-after-listing-2015-2020/. Accessed February 18, 2026.« Back to 2022 American Transplant Congress