Racial and Immunologic Disparities Impact Access to Repeat Kidney Transplantation Among Patients with Previous Failed Kidney Allograft
1Emory University, Atlanta, GA, 2University of Minnesota, Minneapolis, MN
Meeting: 2022 American Transplant Congress
Abstract number: 514
Keywords: African-American, Kidney, Organ Selection/Allocation, Retransplantation
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Name: Health Equity and Access II
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:30pm-6:40pm
Presentation Time: 6:30pm-6:40pm
Location: Hynes Ballroom C
*Purpose: The number of patients with a failed kidney transplant who are being considered for retransplantation is increasing steadily. However, disparities in access to repeat waitlisting and retransplant have not been well described.
*Methods: We examined a cohort of 81,818 patients with a failed kidney transplant in the United States Renal Data System (1995-2018), and assessed access to repeat wait-listing and repeat transplantation.
*Results: Approximately half of the study population was re-listed after graft failure, including similar proportions of white (50.2%), and Black (47.6%), and Hispanic patients (49.5%); in sociodemographic/clinical adjusted analyses, there were no differences in re-waitlisting of Black patients (HR 0.98; 95% CI: 0.96, 1.01). Although race/ethnicity
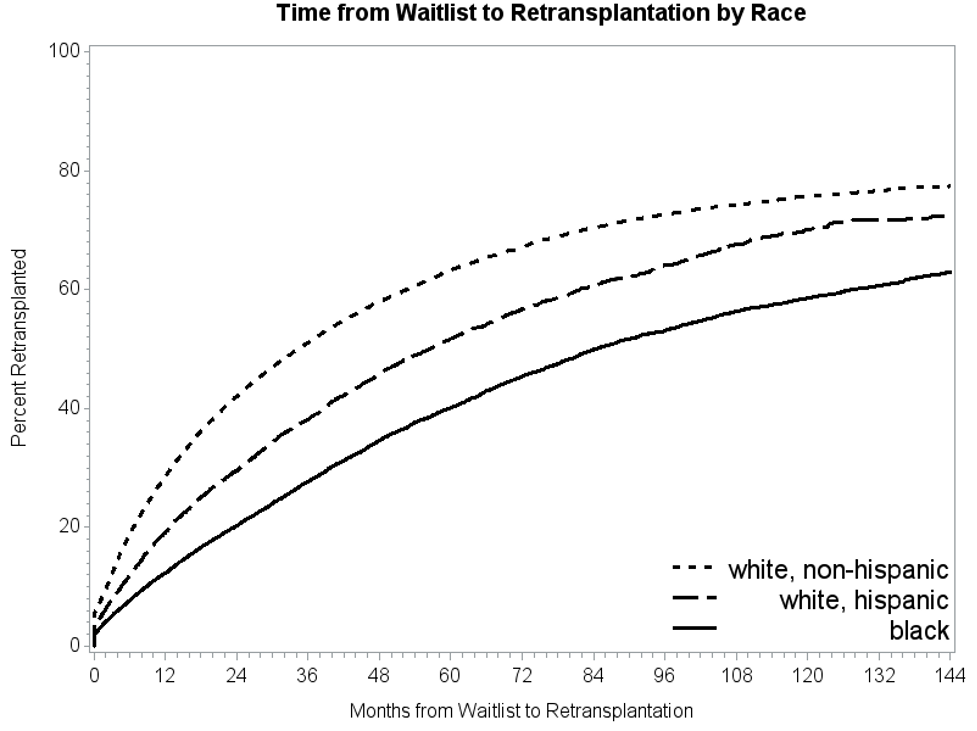
had little influence on whether a patient was re-waitlisted, race/ethnicity demonstrated a significant impact on the likelihood of retransplant. When controlling for all covariates, Both Black (HR 0.65, 95% CI: 0.63, 0.68) and Hispanic (HR 0.83; 95% CI: 0.79-0.87) patients had a lower likelihood of retransplant than white patients. The median time from graft failure to retransplantation was 26.6 months (IQR: (10.7, 52.9 months; however, this waiting time varied by race: among Black patients, the median time was 40.8 months (IQR: 18.7-69.5 months) months versus 20.5 months (IQR: 8.3-42.0 months) among white patients.When stratified by recipient PRA, racial disparities were reduced; however, moderate and highly sensitized Black and Hispanic patients had reduced access to retransplant from the waiting list. Black and Hispanic patients were less likely to undergo repeat kidney transplant at any PRA level compared to white patients, and that this disparity was exacerbated in the low-moderately sensitized and highly patients. In fact, highly sensitized (PRA>80) Black patients were almost half as likely to receive a deceased donor transplant (HR 0.63, p<0.001) relative to highly sensitized white patients despite the same PRA category.
*Conclusions: In this study, patient race was not a factor in access to the waitlist among patients awaiting repeat transplantation, but does have a significant impact on the likelihood of receiving a repeat transplant while on the waitlist. Further, immunologic disparities play a significant role in access to repeat kidney transplantation. Policies and strategies addressing both sociodemographic and immunologic disparities that should be promoted to improve access to kidney retransplant for minority patients.
To cite this abstract in AMA style:
Lovasik BP, Zhang R, Lynch R, Patzer R, Adams A. Racial and Immunologic Disparities Impact Access to Repeat Kidney Transplantation Among Patients with Previous Failed Kidney Allograft [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/racial-and-immunologic-disparities-impact-access-to-repeat-kidney-transplantation-among-patients-with-previous-failed-kidney-allograft/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress