Race-Based Differences in Simultaneous Liver and Kidney Transplant Utilization and Outcomes
1Department of Internal Medicine, University of California San Francisco, San Francisco, CA, 2University of California San Francisco, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 129
Keywords: Kidney/liver transplantation, Resource utilization, Waiting lists
Topic: Clinical Science » Liver » 52 - Liver: Kidney Issues in Liver Transplantation
Session Information
Session Name: Cirrhosis: Complications, Portal Hypertension and Renal Management
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:40pm-6:50pm
Presentation Time: 6:40pm-6:50pm
Location: Hynes Room 311
*Purpose: Race-based variations in rates of kidney dysfunction exist. We aimed to understand the utilization and impact of simultaneous liver-kidney transplantation (SLKT) by race.
*Methods: Patients self-identified as Black (B), Asian/Other (A), White (W). We performed trend analyses on adults listed for primary liver transplantation (LT) from 2008 – 2018 in the UNOS registry. Logistic regression tested the association between race and SLKT listing. Competing risk models tested the association between race and waitlist mortality. Cox models tested the association between race and post-LT mortality.
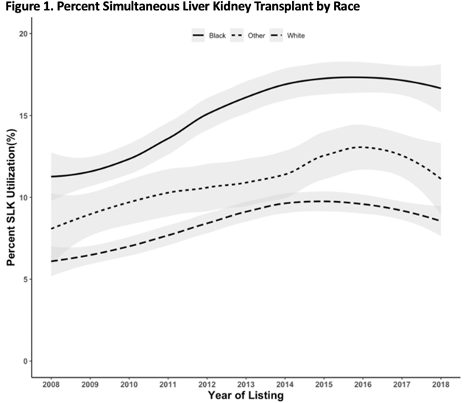
*Results: Of 117,275 patients listed for LT, more Black patients were listed for SLKT (B 15% v. W 8% v. A 11%, p<0.001). SLKT listing is increasing at a greater rate among Blacks (B 0.70% per year v. W 0.34% per year v. A 0.42% per year, p<0.001) (Figure 1). Listing: Among the 117,275 waitlist registrants, Black race was associated with SLKT listing (odds ratio [OR] 2.79, p<0.001), and this association (aOR 2.11, p<0.001) persisted after controlling for age, ascites, hepatic encephalopathy, MELD-Na, diabetes (DM), acute kidney injury (AKI), chronic kidney injury (CKD), and cirrhosis etiology. Compared to White patients with the same diagnoses and controlling for confounders, Black patients with hepatitis C (HCV), CKD, or DM were significantly more likely to be listed for SLKT. Waitlist mortality: Among the 9,310 patients listed for SLKT and as compared to White patients, Black patients were not associated with waitlist mortality (sub hazard ratio [HR] 0.91; p=0.10). Post-LT mortality: Among the 6,358 patients who underwent SLKT, post-SLKT mortality occurred in 28% B, 24% W, and 21% A (p<0.001). Compared to White patients, Black patients had higher overall post-SLKT mortality (HR 1.23, p=0.003), and this persisted (HR 1.21, p=0.007) after controlling for age, MELD-Na, sex, etiology, DM, AKI, CKD, and donor risk index. Compared to White patients with the same diagnoses and controlling for confounders, Black patients with alcohol related liver disease or HCV were significantly more likely to die post-SLKT.
*Conclusions: Black patients experienced an increasingly greater utilization of SLKT and worse post-SLKT outcomes. Our data suggest that HCV, CKD, and DM statuses impact the race-based disparities in SLKT utilization and cirrhosis etiology impacts post-SLKT survival. These race-based disparities highlight a need to address race-based modifiable risk factors (e.g., HCV, DM) to optimize SLKT utilization and post-LT outcomes.
To cite this abstract in AMA style:
Subbaraj L, Lai J, Cullaro G. Race-Based Differences in Simultaneous Liver and Kidney Transplant Utilization and Outcomes [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/race-based-differences-in-simultaneous-liver-and-kidney-transplant-utilization-and-outcomes/. Accessed February 17, 2026.« Back to 2022 American Transplant Congress