Race, Admissions, and Renal Transplant Waitlisting.
Surgery, Emory University, Atlanta, GA
Meeting: 2017 American Transplant Congress
Abstract number: D291
Keywords: Allocation, Kidney transplantation, Public policy, Waiting lists
Session Information
Session Name: Poster Session D: Non-Organ Specific: Economics, Public Policy, Allocation, Ethics
Session Type: Poster Session
Date: Tuesday, May 2, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Background: We have previously shown that increased hospitalization while listed for renal transplantation is associated with excess waitlist mortality, reduced odds of transplantation, and inferior recipient and graft survival. We sought to determine whether patterns of baseline admissions might be used to identify incident ESRD patients with potential for good waitlist and transplant outcomes.
Methods: We used United States Renal Data Systems files to perform a retrospective review of all adult new-onset ESRD cases, limited to individuals with primary Medicare coverage over the first 6 months after ESRD onset to capture number of days spent inpatient. Socioeconomic status was approximated by ZIP code poverty rate. Cox multivariable analysis was performed to determine impact of demographics, comorbidities and hospitalization history on survival and successful transplant listing.
Results: A total of 470,084 patients were studied. EPTS score at ESRD onset was lower in black than white patients, and higher among those in poorer areas. The overall rate of waitlisting was 11.8% for white and 5.3% for black patients. Baseline admissions reduced likelihood of waiting approximately equally by race, but the ratio of white to black patients listed was significantly greater among more-heavily admitted groups (figure 1). In multivariable Cox modeling, >20% poverty by ZIP code was associated with decreased likelihood of waitlisting (HR 0.754, 95% CI 0.734-0.776). Black patients who were never listed had superior survival to white patients at each level of admissions (3 year survival 75.2% vs. 67.2% for non-admitted patients, 53.2% vs. 45.9% for patients with 15+ days inpatient, p < 0.0001 for both comparisons). Excess admissions significantly reduced likelihood of listing (HR for 15+ days 0.753 (95%CI 0.732-0.774)) and increased likelihood of death among non-listed patients (HR 1.58 for 15+ days (95% CI 1.57-1.60)). 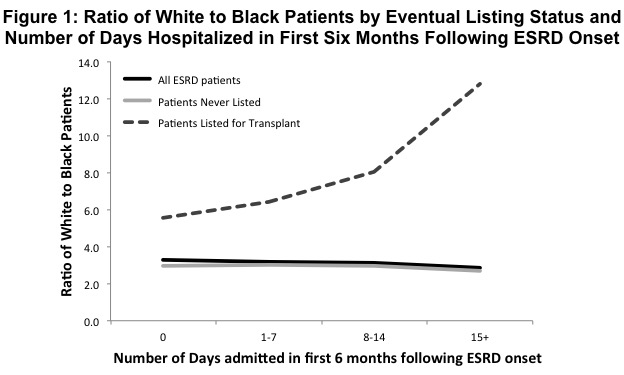 Conclusions: Black ESRD patients are less likely to be waitlisted than whites, especially in the setting of high baseline admissions. Use of admissions as a candidate performance metric could improve disparities in access to the waitlist for black patients and extend the utility of the organ supply.
Conclusions: Black ESRD patients are less likely to be waitlisted than whites, especially in the setting of high baseline admissions. Use of admissions as a candidate performance metric could improve disparities in access to the waitlist for black patients and extend the utility of the organ supply.
CITATION INFORMATION: Lynch R, Zhang R, Patzer R, Larsen C, Adams A. Race, Admissions, and Renal Transplant Waitlisting. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Lynch R, Zhang R, Patzer R, Larsen C, Adams A. Race, Admissions, and Renal Transplant Waitlisting. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/race-admissions-and-renal-transplant-waitlisting/. Accessed February 17, 2026.« Back to 2017 American Transplant Congress
