Psychotic Disorders and Outcomes after Kidney Transplantation
M. Molnar,1,2 J. Eason,1,2 A. Gaipov,3 M. Talwar,1,2 P. Potukuchi,3 K. Kalantar-Zadeh,4 C. Kovesdy.3,5
1Division of Transplant Surgery, Methodist University Hospital Transplant Institute, Memphis, TN
2Department of Surgery, University of Tennessee Health Science Center, Memphis, TN
3Division of Nephrology, Department of Medicine, University of Tennessee Health Science Center, Memphis, TN
4Division of Nephrology, University of California, Irvine, CA
5Nephrology Section, Memphis Veterans Affairs Medical Center, Memphis, TN.
Meeting: 2018 American Transplant Congress
Abstract number: B189
Keywords: Kidney transplantation, Outcome, Psychiatric comorbidity
Session Information
Session Name: Poster Session B: Kidney Psychosocial
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Background: The prevalence of bipolar disorder and schizophrenia combined is around 1-4% in the general population and both represent relative contraindications for kidney transplantation. However, the published data on post-transplant outcomes in patients with pre-transplant psychotic disorders are extremely limited.
Methods: We examined 3,680 US veterans who underwent kidney transplantation (including 717 preemptive transplantation) between 10/2007 and 09/2011. The diagnosis of either psychotic disorder was based on a validated algorithm. Measured confounders were used to create a propensity score-matched cohort. Associations between psychotic disorders and graft loss-censored death, all-cause death and death-censored graft loss were examined in Cox proportional hazard and competing risk regression models.
Results: The mean±SD age of the cohort at baseline was 61±11 years, 92% were male, 66% and 27% of patients were white and black, respectively, 72% were married, 48% of the patients were diabetic. Compared to patients without psychotic disorders, psychotic patients had similar graft loss-censored mortality risk in competing risk regression model [Sub-Hazard Ratio (SHR) (95% CI): 0.78 (0.36-1.69)]. Additionally, psychotic patients had similar all-cause mortality risk using Cox regression [HR (95% CI): 0.91 (0.45-1.86)]. Finally, compared to patients without psychotic disorders, psychotic patients had similar death censored graft loss risk using competing risk regression model [SHR (95% CI): 1.00 (0.42-2.37)]. Similar results were found in different subgroups. 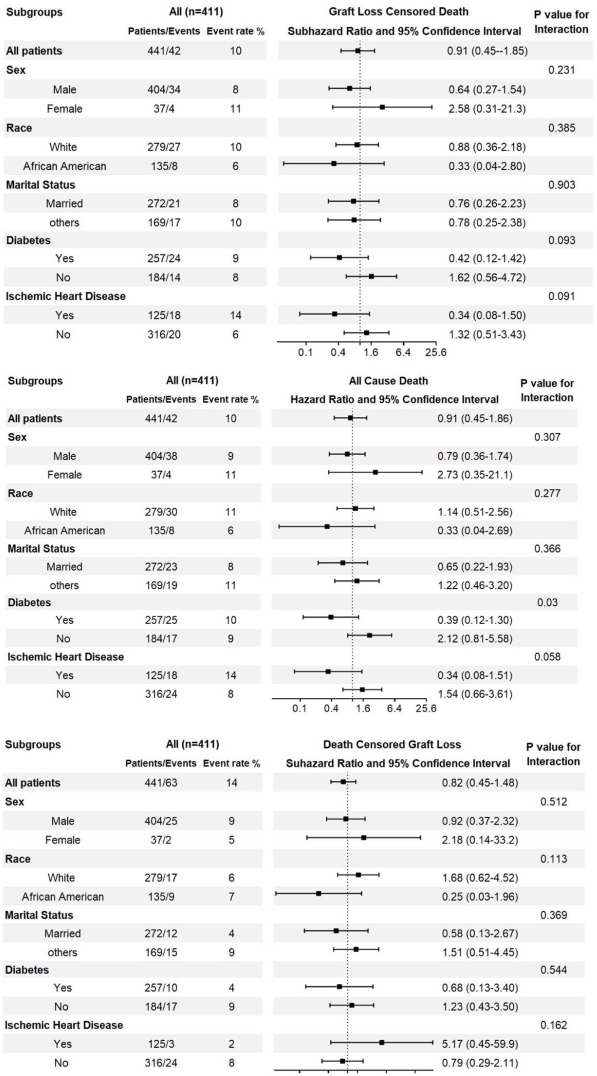
Conclusions: Psychotic disorders are not associated with adverse outcomes in kidney transplant recipients.
CITATION INFORMATION: Molnar M., Eason J., Gaipov A., Talwar M., Potukuchi P., Kalantar-Zadeh K., Kovesdy C. Psychotic Disorders and Outcomes after Kidney Transplantation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Molnar M, Eason J, Gaipov A, Talwar M, Potukuchi P, Kalantar-Zadeh K, Kovesdy C. Psychotic Disorders and Outcomes after Kidney Transplantation [abstract]. https://atcmeetingabstracts.com/abstract/psychotic-disorders-and-outcomes-after-kidney-transplantation/. Accessed February 16, 2026.« Back to 2018 American Transplant Congress
