Primary Uretero-ureterostomy in Renal Transplantation
1Advanced Surgery, John C. McDonald Regional Transplant Center - Willis Knighton Health System, Shreveport, LA, 2Transplant Nephrology, John C. McDonald Regional Transplant Center - Willis Knighton Health System, Shreveport, LA, 3Urology, John C. McDonald Regional Transplant Center - Willis Knighton Health System, Shreveport, LA
Meeting: 2021 American Transplant Congress
Abstract number: 378
Keywords: Kidney transplantation, Outcome, Surgical complications
Topic: Clinical Science » Organ Inclusive » Surgical Issues (Open, Minimally Invasive):All Organs
Session Information
Session Name: Surgical Issues and Deceased Donor Management
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 8, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:20pm-6:25pm
Presentation Time: 6:20pm-6:25pm
Location: Virtual
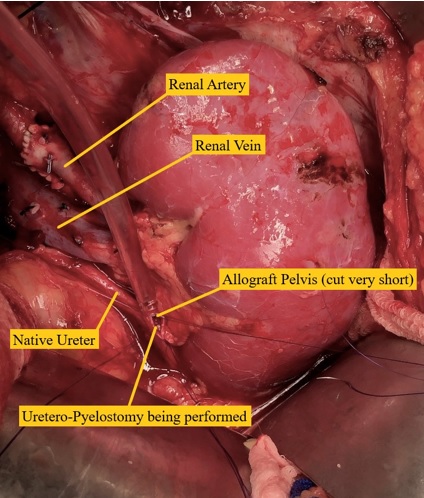
*Purpose: Uretero-neocystostomy (UN) is routinely performed in renal transplantation. Few studies of primary uretero-ureterostomy (UU) have been reported, showing its safety and feasibility. If the ureter is inadvertently cut short during procurement, the organ can still be used with UU or uretero-pyelostomy, avoiding discard. We started UU technique in 2016 to avoid the need for secondary UU. The aim of this study was to compare the incidence of urological complications and graft & patient survival between the two techniques.
*Methods: From Jan 2009 to Aug 2020, we studied patients with Kidney (KT), Kidney-Pancreas (KPT), and Liver-Kidney (LKT) transplantation. Exclusion criteria included reflux as the cause of ESRD, en-block-KT, patients lost to followup before 5 years, and graft failure within 10 days. Data was collected on patient demographics, peri-operative findings, incidence of urine leak, stricture and fluid collection, and death-censored 5-year graft & patient survival. Categorical variables with Chi-Square test, continuous variables with Student’s T-test, and survival analysis with Log Rank test were done using SPSS.
*Results: Among 515 patients (KT=405, KPT=91, LKT=19), 190 had UU and 325 had UN. 4 patients were converted to UN intraoperatively due to atrophic ureter. In those who underwent UN, 6 patients required secondary UU. There was no statistically significant difference in incidence of urological complications. Foley catheter was taken out earlier and ureteral stricture developed earlier in UU patients (2.3 ± 1.5 vs 18.0 ± 22.9 months, p-value = 0.03). In KT, OR time was shorter in UU (2:39 vs 2:57, p-value = 0.05), and in KPT, death-censored 5-year graft survival rate was better in UU patients (100% vs 75.5%, p-value = 0.04).
| Total UU (n=190) | Total UN (n=325) | P-Value | KT UU (n=136) | KT UN (n=269) | P-Value | |
| Age (Y), mean ± SD | 48.5 ± 13.2 | 47.8 ± 0.52 | 0.52 | 49.5 ± 13.7 | 48.5 ± 12.5 | 0.42 |
| Male, % (n) | 61.1 (116) | 57.5 (187) | 0.43 | 61.0 (83) | 56.9 (153) | 0.42 |
| Foley Catheter Duration (d), mean ± SD | 4.0 ± 2.4 | 4.9 ± 2.1 | 0.01 | 4.0 ± 2.5 | 4.5 ± 1.5 | 0.17 |
| Incidence of Leak, % (n) | 1.6 (3) | 0.6 (2) | 0.28 | 2.2 (3) | 0.7 (2) | 0.21 |
| Incidence of Stricture, % (n) | 1.6 (3) | 2.5 (8) | 0.50 | 0.7 (1) | 2.2 (6) | 0.28 |
| Incidence of Fluid Collection, % (n) | 1.6 (3) | 0.3 (1) | 0.11 | 2.2 (3) | 0.4 (1) | 0.08 |
| 5-Year Death-Censored Graft/Patient Survival, % | 96.8/93.2 | 89.2/92.9 | 0.49/0.06 | 95.6/93.4 | 91.4/92.2 | 0.46/0.23 |
*Conclusions: UU is safe and easy to perform with comparable long-term results and has advantages of shorter OR time, removing Foley catheter earlier, and preventing organ discard and secondary UU.
To cite this abstract in AMA style:
Shokouh-Amiri H, Naseer MS, Aultman D, McMillan R, Tandukar S, Siskron FT, Singh N, Zibari G. Primary Uretero-ureterostomy in Renal Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/primary-uretero-ureterostomy-in-renal-transplantation/. Accessed February 19, 2026.« Back to 2021 American Transplant Congress