Pregnancy After Heart Transplant Does Not Negatively Impact Long Term Patient Survival
1Surgery, Lehigh Valley Health Network, Allentown, PA, 2Cardiovascular Medicine, University of South Florida, Morsani College of Medicine, Tampa, FL, 3Data Analytics, University of South Florida, Muma College of Business, Tampa, FL, 4Transplant Pregnancy Registry International, Philadelphia, PA, 5Nephrology, University of Virginia Health System, Charlottesville, VA, 6Medicine, Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Meeting: 2022 American Transplant Congress
Abstract number: 146
Keywords: Heart transplant patients, Pregnancy, Quality of life, Survival
Topic: Clinical Science » Heart » 63 - Heart and VADs: All Topics
Session Information
Session Name: Heart and VADs: All Topics I
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:30pm-6:40pm
Presentation Time: 6:30pm-6:40pm
Location: Hynes Room 210
*Purpose: To evaluate the impact of pregnancy on patient survival in heart transplant recipients (HTRs), we linked the Transplant Pregnancy Registry International (TPRI) dataset with the Scientific Registry of Transplant Recipients (SRTR) and compared outcomes in HTRs with and without post-transplant pregnancies.
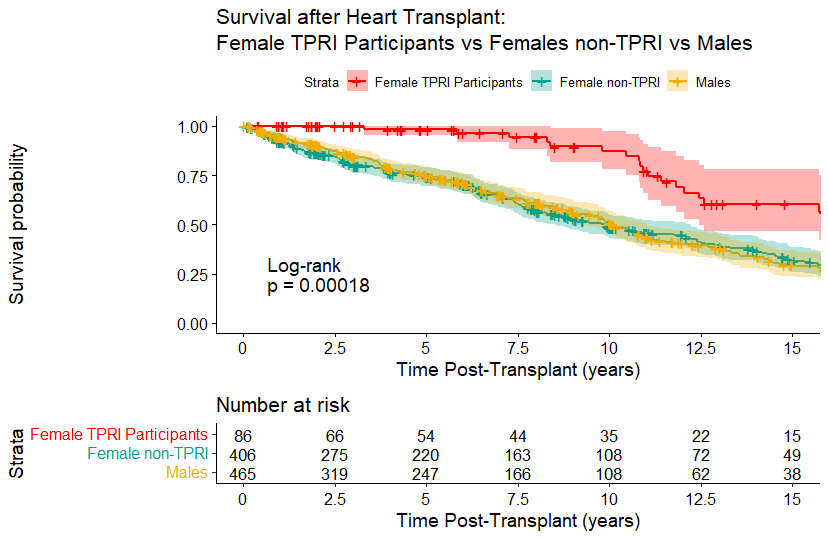
*Methods: The linkage of databases was IRB approved. Of the 115 women with pregnancies after HT in TPRI, 88 were identified in SRTR dataset by linking key variables. A comparative cohort of 10:1 HTRs matched for age at transplant and year of transplant was pulled from SRTR’s >70,000 recipients. Demographic variables were analyzed by X2 or Fisher’s Exact Test, survival by Kaplan-Meier (KM) and Cox proportional hazards and differences assessed by log rank test. Analysis was performed in R version 4.0.4.
*Results: Comparing demographics of TPRI vs SRTR controls, the only difference was TPRI cohort skewed towards white race. For the SRTR cohort KM survival showed that females had the same survival as age-matched males (p=0.89, log rank test). For both genders, race had a significant impact on survival, i.e., white race was associated with higher long-term survival (p<0.0009). Time was examined by splitting the female group into quintiles by transplant year. The earliest (1987-91) and the most recent (2011-21) had slightly longer survival (log rank 0.00034). TPRI cohort was proportionately represented across quintiles, p=0.9 (X2). TPRI participants had higher long-term survival compared with female non-participants and compared with males (p=0.00018). This effect was independent of transplant year (p=0.06).
*Conclusions: Prior TPRI analyses of pregnancy in HTRs have shown acceptable patient, graft, and pregnancy outcomes. Here, we show that HTRs with a history of pregnancy had longer survival compared to age and transplant year-matched HTRs. It is likely that natural selection of healthier HTRs embarking on pregnancy accounts for the difference. Overrepresented white race in the TPRI cohort is a potential cofounder. Despite the limitations of the study, these data support the safety of pregnancy in heart transplant recipients.
To cite this abstract in AMA style:
Moritz MJ, Lee D, Madu C, Hossain S, Coscia LA, Rao S, Constantinescu S. Pregnancy After Heart Transplant Does Not Negatively Impact Long Term Patient Survival [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/pregnancy-after-heart-transplant-does-not-negatively-impact-long-term-patient-survival/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress