Predictors of Poor Outcomes Following Liver Transplantation in Patients with Hepatopulmonary Syndrome
Division of Liver and Pancreas Transplantation, The Dumont-UCLA Liver Transplant Center, Los Angeles, CA
Meeting: 2013 American Transplant Congress
Abstract number: A596
Purpose. Orthotopic liver transplantation (OLT) is the only effective therapy for chronic liver disease patients with hepatopulmonary syndrome (HPS). Recent reports have documented improved long-term survival but excess complication rates among patients with HPS undergoing OLT. The purpose of the current study is to identify predictors of poor outcomes in HPS patients following liver transplantation.
Methods. We retrospectively reviewed a cohort of 26 patients who were granted Model for Endstage Liver Disease (MELD) exception points for HPS and underwent OLT at our center between July 2003 and February 2012, with a median follow-up of 5.2 years. Overall survival and complications were analyzed in relation to preoperative clinical variables, arterial oxygen tension (PaO2) measurements, and pulmonary function testing values.
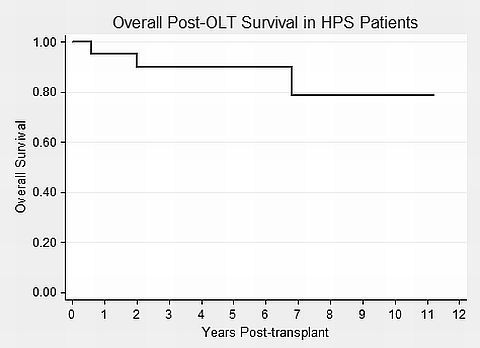
Results. Overall mortality in this study was 7/26 (27%; Figure), with a perioperative mortality rate of 4/26 (15%). The most common cause of death was severe sepsis resulting in multiple organ dysfunction (4/26; 15%).
Hypoxic respiratory failure was the most frequent postoperative complication, occurring in 6/26 (23%) of recipients. Other complications were mostly infectious (4/26, 15%), and vascular or hemorrhagic (2/26, 8%) in nature. On regression analysis, preoperative diffusion lung capacity for carbon monoxide (DLCO) was most predictive of peri-transplant morbidity (OR=0.88, P=0.03). The mean ± SE % of predicted DLCO was 35.3 ± 2.8% among patients with complications vs. 56.5 ± 5.7% among those without. Of note, all 4 patients in the study cohort with coexisting pulmonary fibrosis and HPS developed complications post-transplantation. Preoperative PaO2, previously thought to be a strong predictor of mortality, was not associated with adverse outcomes in the current study.
Conclusions. Liver transplantation in patients with HPS carries significant morbidity. Severely decreased DLCO on preoperative pulmonary function testing portends a poor prognosis, and careful consideration should be used when evaluating this subgroup of patients for transplantation.
To cite this abstract in AMA style:
Cheng E, Zopey R, Wang T, Busuttil R. Predictors of Poor Outcomes Following Liver Transplantation in Patients with Hepatopulmonary Syndrome [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/predictors-of-poor-outcomes-following-liver-transplantation-in-patients-with-hepatopulmonary-syndrome/. Accessed February 16, 2026.« Back to 2013 American Transplant Congress
