Predictors of Clostridium Difficile Infection in Liver Transplant Recipients: A 10 Year Single-Center Cohort Study
Transplant Institute, Henry Ford Hospital, Detroit, MI
Meeting: 2013 American Transplant Congress
Abstract number: B1051
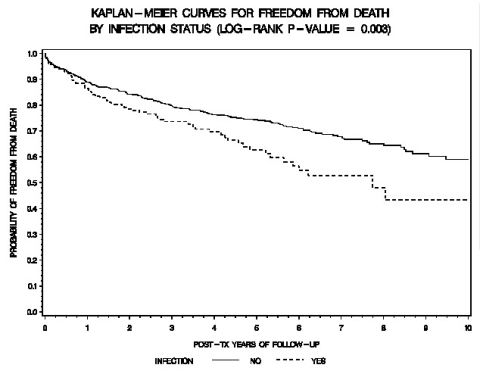
Background: Clostridium difficile infection (CDI) is a common cause of morbidity and is associated with increased in-hospital mortality among solid organ transplant recipients. The incidence of CDI in liver transplant recipients (LTR) is 3-7%. Data on the recent epidemiology, predictors of CDI, recurrence rates, and outcomes of CDI in LTR is limited. Methods: A 10-year retrospective cohort study was performed of all LTR (2000-2010) at a tertiary care hospital. CDI was defined as a LTR with diarrhea and a stool C. difficile toxin positive test. Data collected included demographics, Charlson’s comorbidity index, MELD score, length of stay, time to CDI, community versus hospital onset CDI, severe CDI (WBC >15,000 cells/mm3), recurrence (≤3 months) and relapse (≤4 weeks) and overall mortality. Predictors of CDI were calculated using Cox proportional hazard model adjusted for age, gender and race. Results: 970 LTR were followed for an mean 5.3 ± 3.4 years. Prevalence of CDI was 19% (n=183). CDI occurred at a median of 51 days post-LT. Severe CDI was diagnosed in 29%. CDI recurrence rate was 16.9%, (mean:62.5± 26.5 days) and relapse rate was 9.7%. Of all patients with CDI, 38% had community-onset. Independent predictors of post-LTR CDI were year of LTR (HR 1.137, 95% CI 1.06-1.22; p<0.001), white race (HR 1.47, 95% CI 1.09-2.1; p=0.035), MELD score (HR 1.03, 95% CI 1.01-1.045, p=0.003) and length of stay (HR 1.01, 95% CI 1.005-1.02, p<0.001). The highest rates of CDI in LTR occurred in 2007-2008, similarly to our general hospital population. Significant mortality was observed among LTR with CDI. Conclusions: CDI is a common complication among LTR associated with significantly overall mortality. Predictors of CDI in LTR, namely the high rates of CDI in the general hospital population, and prolonged length of stay are indicative of nosocomial acquisition of C. difficile. Aggressive detection and treatment of CDI in both inpatient and outpatient LTR is needed to improve outcomes. Meticulous infection control measures including antibiotic stewardship is essential to reduce CDI.
To cite this abstract in AMA style:
Mittal C, Arshad S, Miceli M, Bajjoka I, Brown L, Abouljoud M, Ramesh M, Alangaden G. Predictors of Clostridium Difficile Infection in Liver Transplant Recipients: A 10 Year Single-Center Cohort Study [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/predictors-of-clostridium-difficile-infection-in-liver-transplant-recipients-a-10-year-single-center-cohort-study/. Accessed February 16, 2026.« Back to 2013 American Transplant Congress
