Predictors of Clostridium difficile Infection and Recurrence among 2,622 Solid Organ Transplant Recipients
Columbia University, New York, NY
Meeting: 2019 American Transplant Congress
Abstract number: A347
Keywords: Infection, Mortality, Recurrence, Risk factors
Session Information
Session Name: Poster Session A: Transplant Infectious Diseases
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Clostridium difficile infection (CDI) is common after solid organ transplant (SOT) and is associated with high morbidity and mortality. We assessed incidence, risk factors and outcomes of CDI among SOT patients at a large multiorgan transplant center.
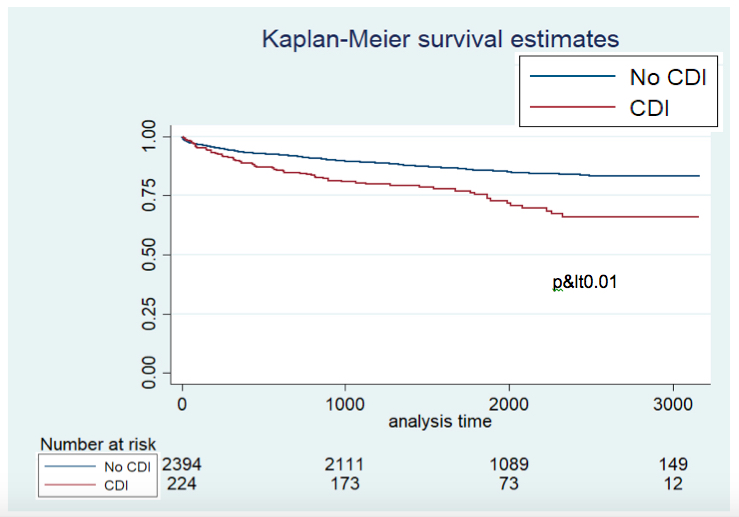
*Methods: All adults with SOT 1/2010-12/2016 at our center were reviewed. CDI was defined as a positive C. difficile PCR within 1 year post-SOT. Multivariate logistic regression was used to identify risk factors for initial and recurrent CDI. The impact of CDI on mortality was assessed with Kaplan Meier curves.
*Results: 2,622 SOT patients were included. 224 (8.5%) patients had CDI 1 year post-SOT. Median age was 58, 59% were male. The highest incidence of CDI was among pancreas recipients (12.5%) followed by lung (11.7%), liver (11.0%), heart (10.8%) and kidney (5.8%). Median time to CDI was 56 days (range 2-354) post-SOT. 64% of patients had severe CDI.
In multivariable regression, significant predictors of post-SOT CDI were recipient age (OR 1.01, p=0.04), days in the ICU (OR 1.01, p<0.01) and organ transplanted when compared with kidney recipients (pancreas OR 2.62, p=0.03, liver OR 2.06, p<0.01, lung OR 2.14, p<0.01, heart OR 1.52, p=0.08). There was an interaction between pre-SOT CDI (OR 4.14, p<0.01) and pre-SOT exposure to high-risk antibiotics (OR 0.70, p=0.05) such that patients with both risk factors had significantly increased odds of CDI post-SOT (OR 5.32, p<0.01).
Among those with CDI, 56.3% were treated with metronidazole, 13.8% oral vancomycin, and 28.6% with both. 31% of patients had recurrent CDI. In multivariable modeling, lung allograft (OR 5.28, p<0.01) was significantly associated with recurrent CDI controlling for age, severe CDI, pre-SOT CDI and oral vancomycin.
Post-SOT CDI was associated with significantly decreased survival (HR 2.03, p<0.01) (Figure1).
*Conclusions: SOT recipients are at high risk for the development of CDI post-transplant and associated with significantly increased mortality. Novel strategies to prevent and effectively treat CDI in SOT are urgently needed.
To cite this abstract in AMA style:
Schluger A, Rosenblatt R, Knotts R, Verna E, Pereira M. Predictors of Clostridium difficile Infection and Recurrence among 2,622 Solid Organ Transplant Recipients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/predictors-of-clostridium-difficile-infection-and-recurrence-among-2622-solid-organ-transplant-recipients/. Accessed March 1, 2026.« Back to 2019 American Transplant Congress