Predictive Validity of Functional Status on Mortality in Adult Kidney Transplant Recipients
N. Chu, Z. Shi, D. Segev, M. McAdams Demarco
Johns Hopkins, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: 550
Keywords: Kidney transplantation, Mortality, Prediction models
Session Information
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:51pm-4:03pm
Presentation Time: 3:51pm-4:03pm
Location: Virtual
*Purpose: Frailty and disabilities, though not routinely measured, are highly prevalent in kidney transplant (KT) recipients and predict poor post-transplant outcomes. The Karnofsky Performance Scale (KPS) is a mandatory, nationally-reported, clinically perceived measure evaluating the ability to manage daily activity. While responses for KPS represent a mixture of gerontological concepts, like frailty, disability, and dependence, little is known about how it relates to these constructs in KT recipients and whether it proves to have predictive validity of adverse post-KT outcomes comparatively.
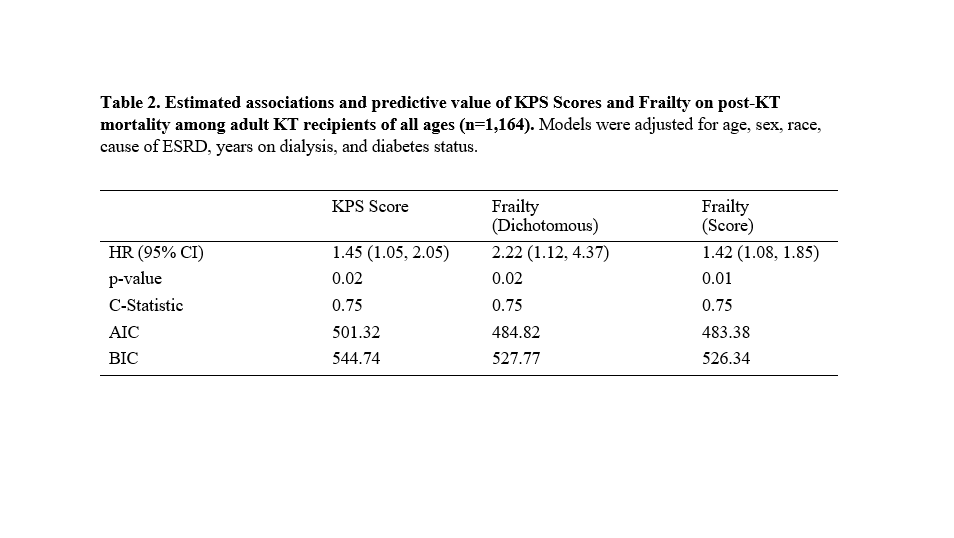
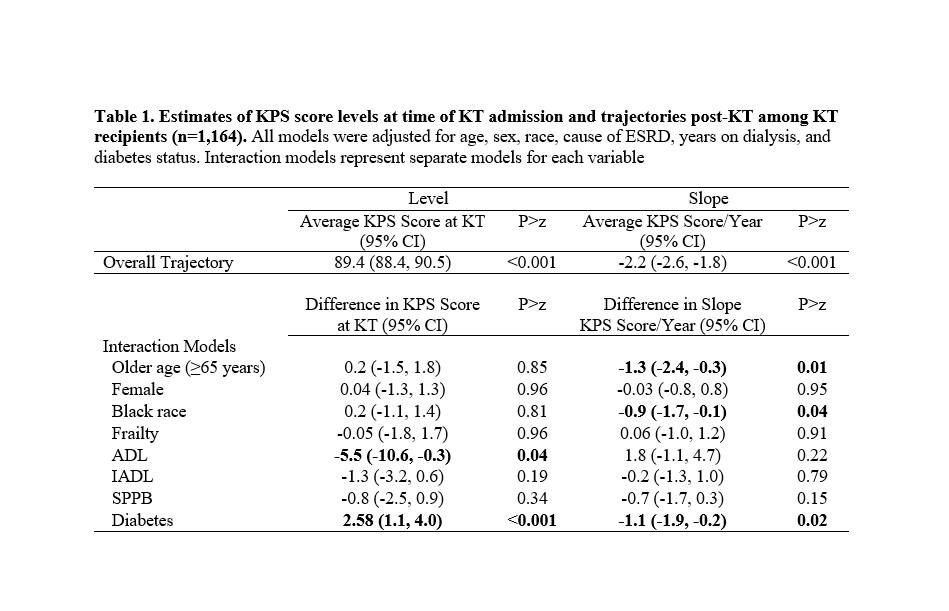
*Methods: Mixed effects models were used to assess KPS trajectories (range 0-100) post-KT in a 2-center cohort study of KT recipients (2009-2018). A Wald test was used to test if slopes differed by age, sex, race, frailty, dependence (ADL/IADL), lower extremity function (SPPB), and diabetes. Model fit (AICs, BICs) and predictive validity (Harrell’s C-statistic) were compared between frailty and KPS on post-KT mortality.
*Results: In 1,164 KT recipients (mean age=52.8), 15.1% were frail, 34.7% had SPPB impairment, and 5.6% had a KPS score≤70%. The average KPS score at KT was 89.4%, and declined at a rate of 2.2%/year. KPS level differed by ADL (difference=-5.5%, 95%CI:-10.6,-0.3) and diabetes (difference=2.58%, 95%CI:1.1,4.0), and KPS slope differed by age (difference=-1.3%/year, 95%CI:-2.4,-0.3), race (difference=-0.9%/year, 95%CI:-1.7,-0.1), and diabetes (difference= –1.1%/year, 95%CI:-1.9,-0.2). Frailty was more strongly related to post-KT mortality compared to KPS; for every 10% reduction in KPS, recipients had 1.45 times greater risk of mortality post-KT, while frail recipients had 2.22 times greater post-KT mortality risk compared to non-frail. Prediction (c-statistics) was equivalent across models, though a model with frailty score appeared to have a better fit (AIC=483.38 BIC=526.34).
*Conclusions: KPS declines post-KT, and declines differ by age, race, and diabetes. Both KPS and frailty have good predictive validity, though frailty is more strongly related to post-KT mortality. Transplant centers should consider implementing comprehensive geriatric assessments that include frailty and physical function in order to improve risk stratification.
To cite this abstract in AMA style:
Chu N, Shi Z, Segev D, Demarco MMcAdams. Predictive Validity of Functional Status on Mortality in Adult Kidney Transplant Recipients [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/predictive-validity-of-functional-status-on-mortality-in-adult-kidney-transplant-recipients/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress