Prediction of ESRD Risk in Living Kidney Donors Through Thirty Years Post-Donation
1Johns Hopkins, Baltimore, MD, 2Scientific Regristry of Transplant Recipients, Minneapolis, MN
Meeting: 2022 American Transplant Congress
Abstract number: 96
Keywords: Kidney
Topic: Clinical Science » Kidney » 39 - Kidney Living Donor: Long Term Outcomes
Session Information
Session Name: Kidney Living Donor: Long Term Outcomes
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:40pm-5:50pm
Presentation Time: 5:40pm-5:50pm
Location: Hynes Room 206
*Purpose: Living kidney donors face increased risk of ESRD, although absolute risk remains low through 20 years postdonation. Informed consent for kidney donation depends on accurate estimates of postdonation ESRD risk.
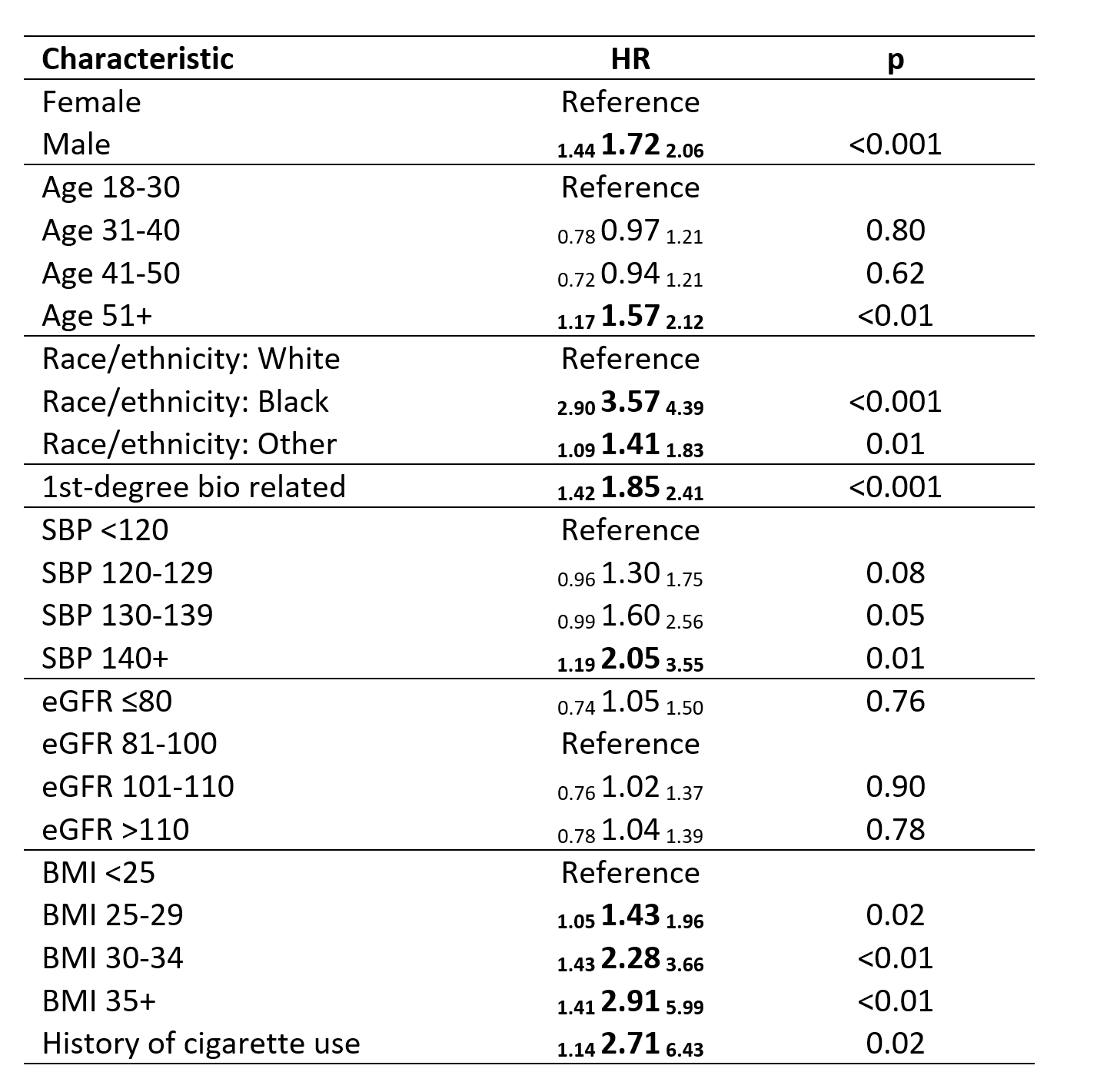
*Methods: Using SRTR data 1987-2020, we modeled the association between donor characteristics and ESRD risk: age, sex, race (White/Black/Other), first-degree biological relationship to recipient, predonation systolic blood pressure, predonation eGFR, and BMI, with multiple imputation to handle missingness. We censored for mortality and fit race-stratified models to investigate interactions.
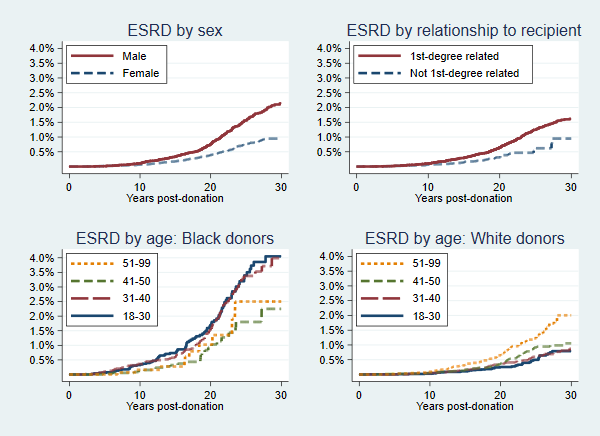
*Results: Among 158,304 donors, 589 experienced ESRD; 1.5% of donors experienced ESRD within 30 years postdonation. 30-year risk of ESRD was higher for first-degree related donors (1.6% vs 0.9%), men (2.1% vs 0.9%), and Black donors (3.6% vs 1.1% White/1.5% Other) (all p<0.01) (Figure). Older age was associated with increased ESRD risk among White donors but decreased risk among Black donors. In multivariate models, higher SBP, BMI>30, and history of cigarette use were associated with increased ESRD risk; predonation eGFR was not associated with risk (Table). The model predicted ESRD risk with C-statistic=0.71.
*Conclusions: ESRD risk through 30 years postdonation varies substantially by donor characteristics, and can be estimated based on predonation characteristics. Donor candidates with high predicted risk should be counseled about their ESRD risk and postdonation behaviors that can delay onset of ESRD.
To cite this abstract in AMA style:
Massie A, Snyder J, Levan M, Brennan D, Al-Ammary F, Segev D. Prediction of ESRD Risk in Living Kidney Donors Through Thirty Years Post-Donation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/prediction-of-esrd-risk-in-living-kidney-donors-through-thirty-years-post-donation/. Accessed February 18, 2026.« Back to 2022 American Transplant Congress