Post‐Donation eGFR Levels Predicts New‐Onset Antihypertensive Medication Use after Living Kidney Donation
1Saint Louis Univ, St. Louis
2Johns Hopkins, Baltimore
3Univ Alberta, Edmonton, Canada
4Western Univ, Ontario, Canada
5Univ Michigan, Ann Arbor
6Lahey Clinic, Burlington
7Hennepin County, Minneapolis
8Symphony Health, Conshohocken
9UCSF, San Francisco.
Meeting: 2018 American Transplant Congress
Abstract number: 335
Keywords: Donation, Glomerular filtration rate (GFR), Hypertension, Outcome
Session Information
Session Name: Concurrent Session: Kidney Living Donor: Long Term Outcomes
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:30pm-5:42pm
Presentation Time: 5:30pm-5:42pm
Location: Room 6A
Limited data are available on the outcome implications of renal function after living kidney donation.
We constructed a novel database linking SRTR registry identifiers, serum creatinine values from an electronic medical records warehouse, and pharmacy fill records for 3,593 living kidney donors (1989–2016) without predonation hypertension per the registry. Estimated glomerular filtration rate (eGFR, ml/min/1.73 m2) was computed from serum creatinine by the CKD-EPI equation. Pharmacy fill capture was assessed within ±90 days of each post-donation lab value, followed by identification of antihypertensive medication (AHM) fills in those with pharmacy records eligibility. A mixed effects model was constructed to assess associations of post-donation eGFR (adjusted odds ratio, 95%LCL aOR 95% UCL) and other baseline factors with AHM treatment requirements after donation.
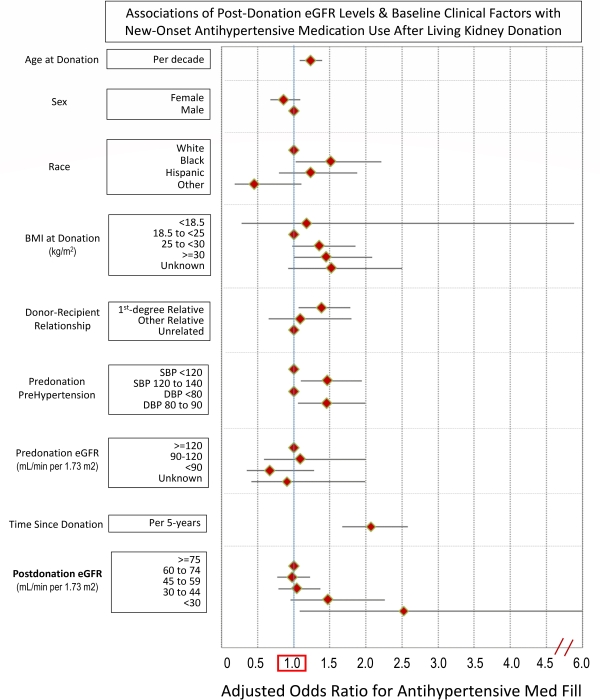
The linked database captured an average of 3 post-donation serum creatinine values per donor (range: 1 to 38). Lower post-donation eGFR bore a graded association with increased AHM use (eGFR 30–44: aOR 0.951.472.26; <30: aOR 1.08 5.902.52). Other significant (P<0.05) correlates of post-donation AHM fills included black race (aOR 2.22), BMI >30 kg/m2 (aOR 2.09), first-degree donor-recipient relationship (aOR 1.79), “pre-hypertension" at donation (SBP 120-139: aOR 1.94; DBP 80-89: aOR 1.99), and longer time since donation. Pre-donation eGFR was not significantly associated with AHM use in the multivariate model.
Lower eGFR levels after living kidney donation are associated with need for AHM treatment. Further work should define relationships of post-donation renal function with renal and cardiovascular morbidity.
CITATION INFORMATION: Lentine K., Segev D., Lam N., Garg A., Naik A., Axelrod D., Xiao H., Henderson M., Massie A., Kasiske B., Hess G., Hsu C., Brennan D., Schnitzler M. Post‐Donation eGFR Levels Predicts New‐Onset Antihypertensive Medication Use after Living Kidney Donation Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Lentine K, Segev D, Lam N, Garg A, Naik A, Axelrod D, Xiao H, Henderson M, Massie A, Kasiske B, Hess G, Hsu C, Brennan D, Schnitzler M. Post‐Donation eGFR Levels Predicts New‐Onset Antihypertensive Medication Use after Living Kidney Donation [abstract]. https://atcmeetingabstracts.com/abstract/postdonation-egfr-levels-predicts-newonset-antihypertensive-medication-use-after-living-kidney-donation/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress