Perioperative Extracorporeal Membrane Oxygenation (ECMO) in Liver Transplantation: A Case Series
1The Dumont-UCLA Transplant Center, UCLA, Los Angeles, CA, 2Cardiovascular Outcomes Research Laboratories, UCLA, Los Angeles, CA, 3Division of Cardiac Surgery, Department of Surgery, UCLA, Los Angeles, CA, 4Department of Anesthesiology, UCLA, Los Angeles, CA
Meeting: 2020 American Transplant Congress
Abstract number: D-134
Keywords: High-risk, Multivisceral transplantation, Retransplantation, Survival
Session Information
Session Name: Poster Session D: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Extracorporeal Membrane Oxygenation (ECMO) is a life-saving treatment modality for patients who develop cardiopulmonary failure refractory to conventional efforts. ECMO has been used sparingly in liver transplantation (LT) over the last 3 decades, with most case reports relegated to its use postoperatively. Additionally, its use in LT remains associated with high mortality. By analyzing ECMO use in the perioperative period, we aimed to understand whether the timing of ECMO cannulation can shed light on its utility in LT.
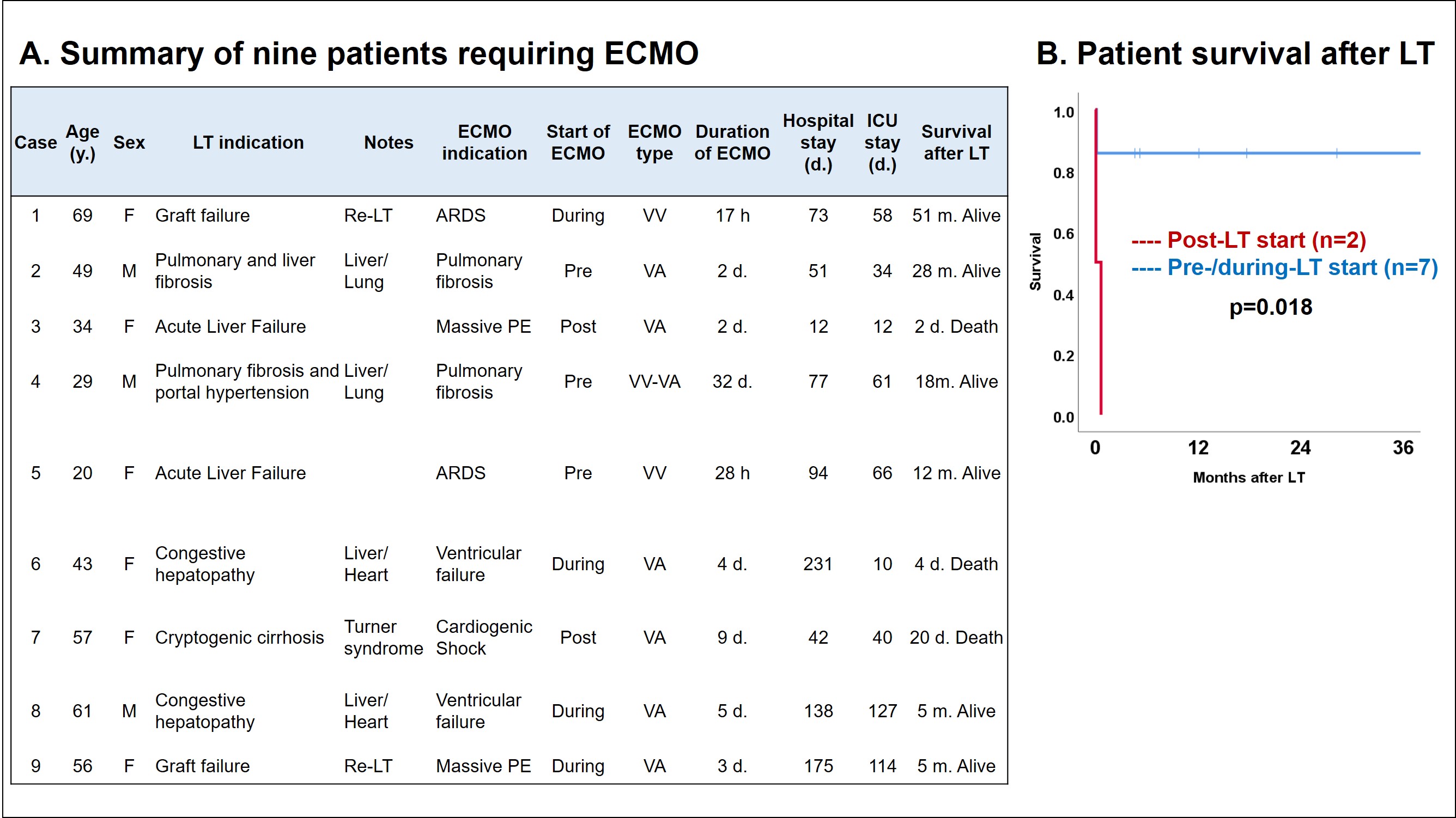
*Methods: This is a retrospective review of 1011 adult LTs from 2012 to 2018. Patients requiring ECMO during the perioperative period were included. Perioperative ECMO use was further categorized according to the start of ECMO cannulation into pre-LT (start in preoperative phase during admission), during-LT (start during LT), and post-LT (start in postoperative phase during admission). Patient characteristics and ECMO data were collected and analyzed.
*Results: Of 1011 LTs, 9 patients received perioperative ECMO [2 Venovenous (VV), 6 Venoarterial (VA), 1 VV-VA]. Of the 9 patients, 2 underwent liver/heart transplant (LHT), 2 underwent liver/lung transplant (LLT), and 2 underwent re-LT [median age: 49 y. , median MELD: 35 (13-42), all donors were DBD donors]. Three patients started ECMO preoperatively (2 for pulmonary fibrosis before liver/lung transplant and 1 for ARDS due to acute liver failure), four started ECMO during LT (1 for massive pulmonary embolism (PE), 2 for ventricular failure during LHT, and 1 for ARDS during re-LT), and two started ECMO postoperatively (1 for post-LT massive PE and 1 for cardiogenic shock in a patient with Turner syndrome). Median hospital/ICU stay was 77/58 days, respectively. While both patients who postoperatively started ECMO died within 1 month of LT, six of seven patients who started ECMO pre-/during-LT achieved 5 months or greater survival after LT (Fig. A, B).
*Conclusions: We report the first case series on perioperative ECMO in LT in the United States. ECMO was associated with excellent long-term survival when used prior to or during transplant, suggesting it can offer the right candidate a bridge through transplantation. In accordance with the literature, however, its use post-LT appears to be more challenging.
To cite this abstract in AMA style:
Guorgui JG, Ito T, Lu MM, Benharash P, Ardehali A, Gudzenko V, Wray C, Agopian VG, III JDiNorcia, Yersiz H, Farmer DG, Busuttil RW, Kaldas FM. Perioperative Extracorporeal Membrane Oxygenation (ECMO) in Liver Transplantation: A Case Series [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/perioperative-extracorporeal-membrane-oxygenation-ecmo-in-liver-transplantation-a-case-series/. Accessed March 1, 2026.« Back to 2020 American Transplant Congress