Percutaneous Direct Intrahepatic Portosystemic Shunt as a Bridge to Liver Transplantation in Pediatric Patients with Variceal Bleeding.
1Department of Surgery, Baylor College of Medicine, Houston, TX
2Department of Radiology, Baylor College of Medicine, Houston, TX
3Department of Pediatrics, Baylor College of Medicine, Houston, TX
Meeting: 2017 American Transplant Congress
Abstract number: B278
Keywords: Infant, Liver cirrhosis, Portal veins
Session Information
Session Name: Poster Session B: Pediatric Liver Transplant - Clinical
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Context: Transjugular intrahepatic portosystemic shunt (TIPS) creation is technically challenging in children due to their small size. The percutaneous direct intrahepatic portosystemic shunt (DIPS) has emerged as an alternative to TIPS in adults, but experience with this technique in children is limited. In this technique, access to the portal vein is gained through ultrasound-guided transhepatic puncture. The shunt is then made directly to the inferior vena cava (IVC) instead of to a hepatic branch (figure 1).
Purpose: To describe our single center experience with percutaneous DIPS as a bridge to liver transplantation in children.
Methods: Between January 2015 and October 2016, 2 patients < 18 years of age underwent percutaneous DIPS creation for variceal bleeding refractory to endoscopic treatment. For the first patient, a 9-month-old 8.9 kg infant with unrepaired biliary atresia, the decision to proceed with percutaneous DIPS instead of TIPS was made due to the small size of the patient. In the second patient, a 12 year-old with congenital liver fibrosis, the decision to proceed with percutaneous DIPS was made after multiple attempts from the right, middle, and left hepatic veins were unsuccessful at TIPS creation due to unfavorable anatomy.
Results: Percutaneous DIPS lowered the portosystemic pressure gradient from 20 mmHg to 11 mmHg in the first case and from 20 mmHg to 13 mmHg in the second case. Neither patient experienced any episodes of variceal bleeding post-DIPS creation. The first patient underwent whole liver transplantation 8 days after shunt creation. The second patient is still waiting for a transplant, with most recent abdominal ultrasound showing patent DIPS 51 days after shunt creation.
Conclusion: Percutaneous DIPS can serve as a life-saving alternative to TIPS in children with challenging anatomy.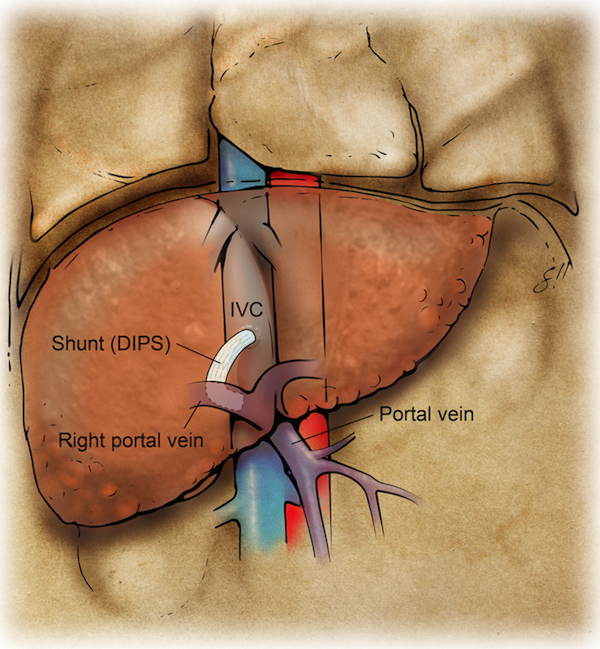
CITATION INFORMATION: Yoeli D, Galvan N, Ashton D, Kumm K, Kueht M, Witte E, Miloh T, Cotton R, Rana A, O'Mahony C, Goss J. Percutaneous Direct Intrahepatic Portosystemic Shunt as a Bridge to Liver Transplantation in Pediatric Patients with Variceal Bleeding. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Yoeli D, Galvan N, Ashton D, Kumm K, Kueht M, Witte E, Miloh T, Cotton R, Rana A, O'Mahony C, Goss J. Percutaneous Direct Intrahepatic Portosystemic Shunt as a Bridge to Liver Transplantation in Pediatric Patients with Variceal Bleeding. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/percutaneous-direct-intrahepatic-portosystemic-shunt-as-a-bridge-to-liver-transplantation-in-pediatric-patients-with-variceal-bleeding/. Accessed February 17, 2026.« Back to 2017 American Transplant Congress
