Pediatric Kidney Transplant Strategy: The Sequence Effect
1Nova Scotia Health Authority Division of Nephrology, Departm, Halifax, NS, Canada, 2Dalhousie University, Halifax, NS, Canada, 3IWK Health Center, Halifax, NS, Canada
Meeting: 2021 American Transplant Congress
Abstract number: 1001
Keywords: Allocation, Kidney transplantation, Living donor, Pediatric
Topic: Clinical Science » Kidney » Kidney Living Donor: Selection
Session Information
Session Name: Kidney Living Donor: Selection
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Improvements in patient survival with pediatric end stage kidney disease (ESKD) predicts needing more than one kidney transplant over a child’s lifetime. Timing of utilization of willing live donor transplant (LD) relative to a deceased donor transplant (DD) remains controversial. Considerations under the current Allocation System notes pediatric DD transplant rates and organ quality are higher than in adults, graft failure rates are higher in adolescent recipients, and smaller children may have transplant hypoperfusion leading to worse graft outcomes. Families perceive benefit to the LD-backup option in case the first DD transplant fails. The best strategy is unclear.
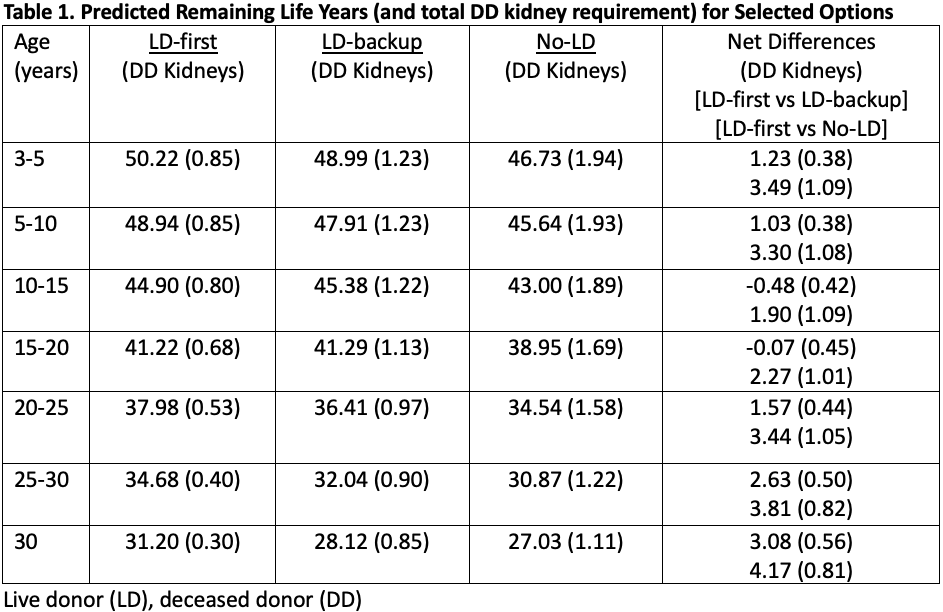
*Methods: Evaluation of 3 transplants over a lifetime, using a Markov model applied to USRDS data, evaluated patient and graft survival. Accounting for reduced transplant candidate eligibility over time and inputting current transplant rates, projected remaining life years (LYs) after transplant were calculated for 3 options: 1) LD-first (LD-DD-DD) with DDs if needed; 2) LD-backup (DD-LD-DD); or 3) No-LD (DD-DD-DD) in recipients age 3 to 30 years.
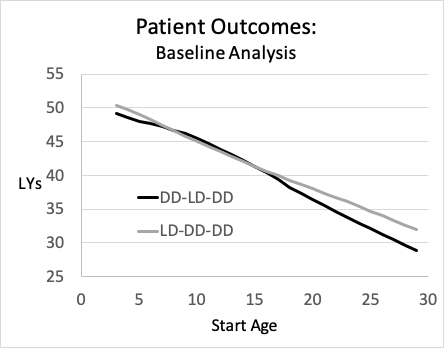
*Results: Opting for a LD-first provided more LYs than the LD-backup option for most recipients (Table 1). The LD-backup sequence was slightly better in recipients age 7 to 15 years, Figure 1. However, the LD-backup advantage disappeared if LD availability changed, candidacy for DD altered (e.g. sensitization), or if pediatric DD transplant rates were lower. The No-LD group produced the fewest LYs for each age category. The Table also shows how many DD organs were used for the 3 options.
*Conclusions: LD-first is best for most pediatric recipients, although LD-backup is slightly better for a subset age 7 to 15 years. Preferential, LD-backup equates to more DD organs utilized by pediatrics and not available for others on the waitlist. Pediatric LD utilization (first or backup) leads to more LYs compared to DD only organ options. The lesson is to ‘utilize LD when you can’.
To cite this abstract in AMA style:
Vinson AJ, Kiberd B, Acott P, Tennankore K. Pediatric Kidney Transplant Strategy: The Sequence Effect [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/pediatric-kidney-transplant-strategy-the-sequence-effect/. Accessed March 1, 2026.« Back to 2021 American Transplant Congress