Outcomes of Hiv-Positive Patients Post-Cardiac Transplantation
1Keck Medicine of USC, Los Angeles, CA, 2University of Arizona Sarver Heart Center, Tucson, AZ, 3UCLA Medical Center, Los Angeles, CA, 4Harbor-UCLA Medical Center, Los Angeles, CA, 5Newark Beth-Israel Medical Center, Newark, NJ
Meeting: 2020 American Transplant Congress
Abstract number: 179
Keywords: Heart transplant patients, HIV virus, Survival
Session Information
Session Name: Heart Transplantation: It's All About the Outcomes
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Human immunodeficiency virus (HIV) infection is no longer an absolute contraindication to heart transplantation (HT) in many HT centers, but long-term post-HT outcomes of HIV+ patients is limited. We sought to obtain more information about the long-term outcomes of HIV+ cardiac transplant recipients.
*Methods: A retrospective analysis of 59,796 HT patients from the United Network Organ Sharing (UNOS) registry from 1987 to 2019 was undertaken. 76 of these patients were HIV+. Characteristics of HT patients with and without HIV were compared using standard statistical methods. Multivariate Cox proportional hazard regression analysis was performed to assess survival outcomes.
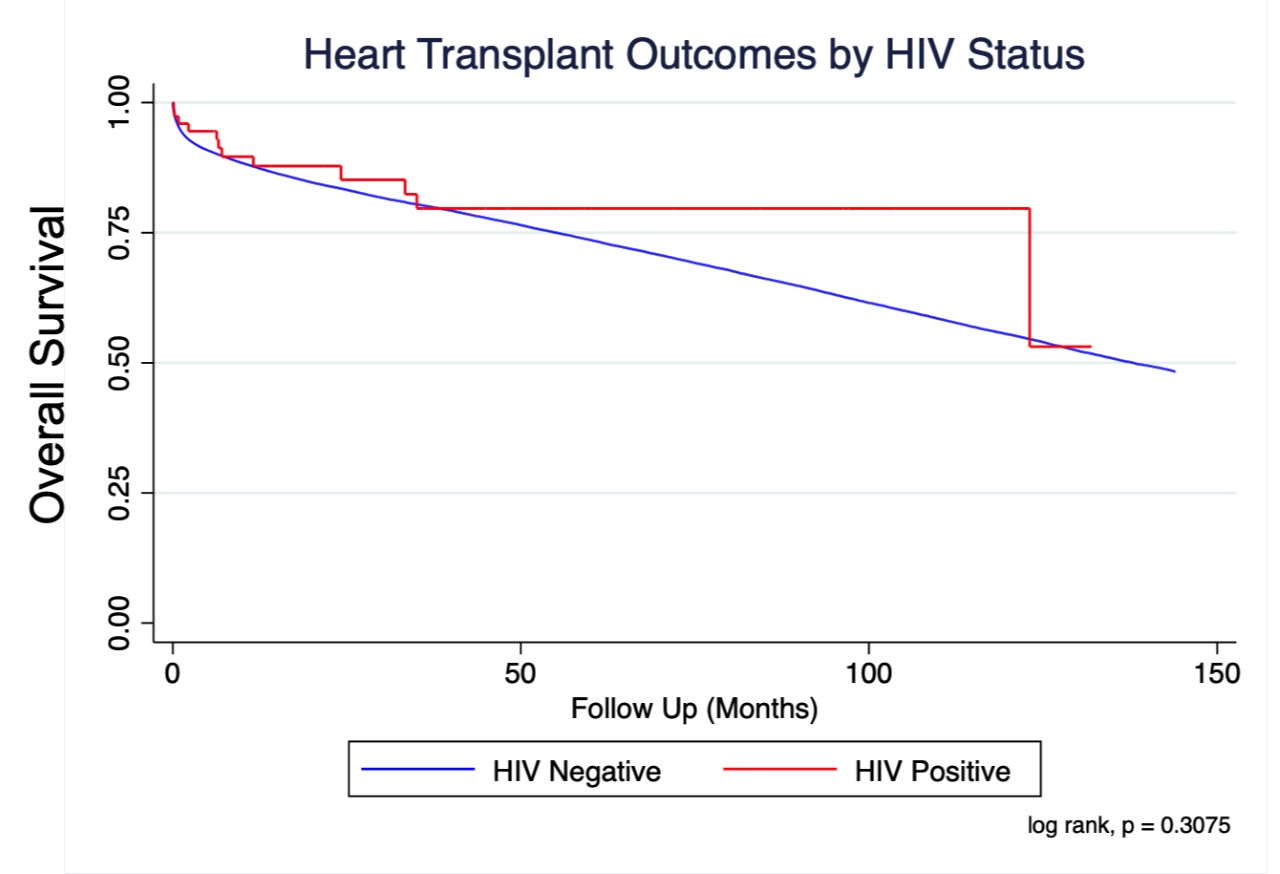
*Results: The mean age and gender division between the HIV+ and HIV- HT recipients were comparable. At time of transplant listing, HIV+ patients were less likely to have undergone prior cardiac surgery (65.8% vs 79.1%, p=0.004). HIV+ recipients had a trend toward receiving older donors (p=0.056), but had similar ischemic times and pulmonary artery catheter measurements. At time of HT, HIV+ patients more frequently required intra-aortic balloon pump (IABP) (11.8% vs 5.5%, p=0.016) and ventricular assist device (VAD) support (47.4% vs 26.7%, p<0.001). The use of extracorporeal membrane oxygenation (ECMO) and mechanical ventilation were similar between the two groups. Median wait time to HT did not differ based on HIV status. There was no statistically significant difference in post-HT survival in a follow-up period of 150 months between the HIV+ and HIV- HT recipients (p = 0.31).
*Conclusions: Long-term post HT survival of HIV+ recipients is comparable to HIV- recipients, despite higher peri-transplant acuity as evidenced by the increased use of IABP and VADs in the former group. HIV status should not preclude carefully selected end-stage heart failure patients from HT consideration. Further study is needed to understand long-term implications of these results.
To cite this abstract in AMA style:
Liu GS, Wolfson AM, Salimbangon AD, Chand RR, Banankhah P, Nattiv J, Genyk PA, Kingsford PA, Li JP, Vucicevic D, Pandya K, Rahman J, Fong M, DePasquale EC, Vaidya AS. Outcomes of Hiv-Positive Patients Post-Cardiac Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-hiv-positive-patients-post-cardiac-transplantation/. Accessed February 24, 2026.« Back to 2020 American Transplant Congress