Outcomes of Donor Nephrectomy (DN) in the Obese.
1Surgery, Univ. of Minnesota, Minneapolis, MN
2Biostatistics and Bioinformatics Core, Masonic Cancer Center, Minneapolis, MN
3Biostatistics, Univ. of Minnesota, Minneapolis, MN.
Meeting: 2016 American Transplant Congress
Abstract number: A142
Keywords: Kidney, Nephrectomy, Obesity, Outcome
Session Information
Session Name: Poster Session A: Kidney Donor Outcomes
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
PURPOSE: In an effort to address the critical organ shortage and rising obesity rates, the criteria for live kidney donation (LKD) have been expanded to include patients with elevated BMI. The association between obesity and the development of diabetes (DM), hypertension (HTN), and end-stage renal disease (ESRD) has raised concerns about the long-term health risks of LKD for obese donors.
METHODOLOGY: All donor and recipient records of DN performed between 1975 and 2014 were reviewed. Donor and recipient demographics, intraoperative parameters, complications, and short- and long-term outcomes were compared between contemporaneous donors with BMI>30 and <30 in a matched-control design.
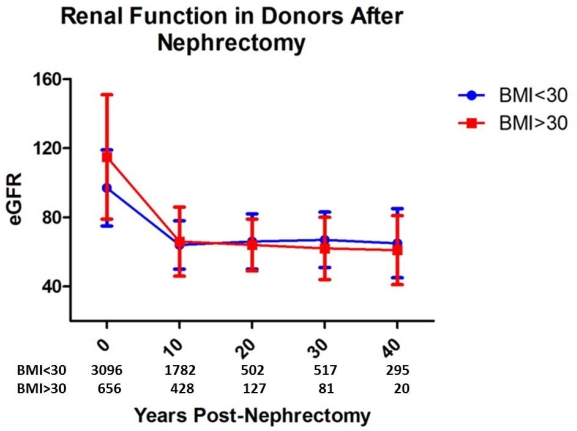
RESULTS: Between 1975 and 2014, we performed 3,752 DN: 2,275 open (ODN), 1,477 laparoscopic DN (LDN). Among donors, 656 (17.5%) had BMI>30. On univariate analysis, BMI>30 donors were more likely to be older (p<0.01), African-American (p<0.01), and smoke at donation (p=0.01). Donation estimated glomerular filtration rate (eGFR) was different between BMI>30 (115+36) and <30 donors (97+22; p<0.001). Intraoperative and post-operative complications were similar among the 2 groups but intraoperative time was longer for BMI>30 donors (p<0.001). Post-operative Length of stay (LOS) was shorter (p=0.03), whereas short-term (<30 days; p<0.01) and long-term (>30 days; p<0.05) readmissions were greater for BMI>30 donors. eGFR (Figure 1) and rates of ESRD were not significantly different >20 years after DN (p=0.71) between BMI>30 and <30 donors. However, long-term development of DM (HR 2.5; 95%CI 1.9-3.4) and HTN (HR 1.3; 95%CI 1.1-1.6) was greater among BMI>30 donors and incidence of disease seemed to occur earlier (diabetes: 12 vs 18 years post-DN; hypertension: 11 vs 15 year post-DN; p<0.001).
CONCLUSION: Obese donors do not appear to be at higher risk for long-term renal function impairment. However, they seem to develop DM and HTN earlier than non-obese donors.
CITATION INFORMATION: Serrano O, Bangdiwala A, Vock D, Minja E, Payne W, Dunn T, Chinnakotla S, Finger E, Pruett T, Matas A, Kandaswamy R. Outcomes of Donor Nephrectomy (DN) in the Obese. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Serrano O, Bangdiwala A, Vock D, Minja E, Payne W, Dunn T, Chinnakotla S, Finger E, Pruett T, Matas A, Kandaswamy R. Outcomes of Donor Nephrectomy (DN) in the Obese. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/outcomes-of-donor-nephrectomy-dn-in-the-obese/. Accessed July 12, 2025.« Back to 2016 American Transplant Congress
