Outcome of Treated Cellular Rejection (CMR) in Renal Transplant Patients
University of Minnesota, Minneapolis, MN
Meeting: 2019 American Transplant Congress
Abstract number: C164
Keywords: Kidney transplantation
Session Information
Session Name: Poster Session C: Kidney: Acute Cellular Rejection
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Prior studies have shown that after treatment of CMR, lack of return to baseline creatinine (Cr.) is associated with increased graft loss. We sought to quantify risk of death censored graft loss (DCGL) by loss of GFR in CMR.
*Methods: We evaluated primary kidney transplant recipients from 2004 – present. We excluded any rejection with AbMR or mixed phenotype. This resulted in 128 first rejection episode: 58 borderline; 27, A1;. 23, 1B; 15,2A; 4,2B; and 1, 3. Methylprednisolone 500mg IV was given for 3 day for borderline, 1a and 1b. Lymphocyte depletional agents were used for any rejection 2A and above or steroid resistant rejection.
Baseline Cr. is defined as nadir Cr. from transplant to one week prior to the rejection episode. Response to treatment was defined as Cr. 30 days from treatment completion. GFR was calculated by CKD- Epi Cr equation. Kaplan Meier curves and COX proportional hazards were calculated for death censored graft loss (DCGL) starting at the time of the first acute rejection treatment. All analysis was performed in R ver. 3.4.3.
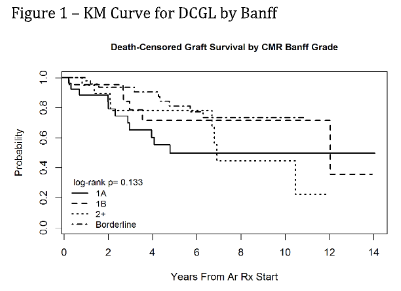
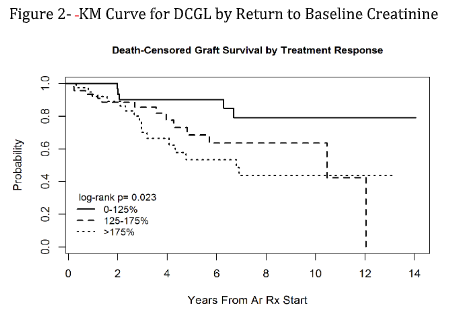
*Results: KM curves for DCGL by Banff grading is shown in fig. 1 and was not statistically significant (p=0.13). KM curves for DCGL by Cr. return to baseline is shown in fig. 2. The closer the Cr. returned to baseline after treatment was associated with improvement in DCGL (p=0.023). A multivariate analysis was performed for DCGL with Cox PH listed in Table 1. Higher baseline GFR was associated with decreased risk such that, for every additional 1 ml/min of GFR prior to rejection, the risk of DCGL decreased by 3.1% (p=0.02). The risk of DCGL increased by 24.4% for every 5ml/ minute GFR loss after treatment (p=0.001). Lastly increase age reduced the risk of DCGL by 4.3% for each year (p=0.001).
*Conclusions: In 128 CMR episodes at a single institution, DCGL hazard ratio increased by 24.4 % for every 5ml/ min of GFR lost. Higher pre rejection GFR and age at time of transplant was protective from DCGL.
To cite this abstract in AMA style:
Raj N, Jackson S, Riad S, Spong R, Vakil V, Matas A, Keys D. Outcome of Treated Cellular Rejection (CMR) in Renal Transplant Patients [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/outcome-of-treated-cellular-rejection-cmr-in-renal-transplant-patients/. Accessed February 8, 2026.« Back to 2019 American Transplant Congress