One-Year Outcomes in Kidney Transplant Recipients with Acute Kidney Injury and COVID-19
P. Shrivastava1, R. M. Hofmann2, S. P. Norman3, D. Granger4, N. Khoury1, R. Prashar1, C. Crombez5, A. Patel1, S. Nagai6, M. Lu7, M. Samaniego1
1Department of Medicine, Henry Ford Health System, Detroit, MI, 2Renal Associates of West Michigan, Grand Rapids, MI, 3Department of Medicine, University of Michigan, Ann Arbor, MI, 4Department of Surgery, Ascension St. John Hospital,, Detroit, MI, 5Department of Transplant Surgery, Henry Ford Health System, Detroit, MI, 6Department of Surgery, Henry Ford Health System, Detroit, MI, 7Department of Public Health Sciences, Henry Ford Health System, Detroit, MI
Meeting: 2022 American Transplant Congress
Abstract number: 971
Keywords: COVID-19, Kidney transplantation, Renal failure, Survival
Topic: Clinical Science » Infection Disease » 24 - All Infections (Excluding Kidney & Viral Hepatitis)
Session Information
Session Name: All Infections (Excluding Kidney & Viral Hepatitis) II
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Acute kidney injury (AKI) occurs in more than half of kidney transplant recipients (KTRs) with COVID-19. The longitudinal trajectory of kidney function is unclear. To study this, we compare mortality outcomes and long-term allograft function as measured by the change in serum creatinine (SCR) after hospital discharge between kidney transplant patients with SARS CoV-2 who experienced in-hospital AKI with who did not have AKI.
*Methods: In this retrospective, multi-center study, we identified 149 KTRs who tested positive for SARS-CoV-2 between March 1st, 2020 and March 31st, 2021. Data from electronic medical records were retrieved and compared between KTRs without AKI and KTRs with AKI who were hospitalized with COVID-19. Creatinine was trended at 0,1,3,6, and 12 months.
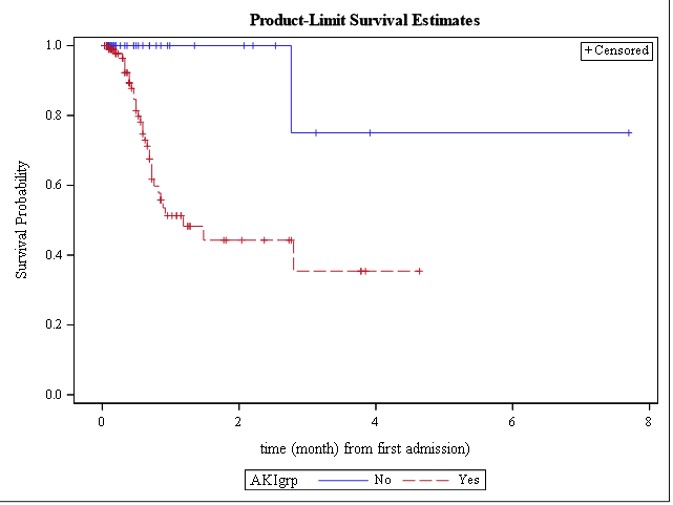
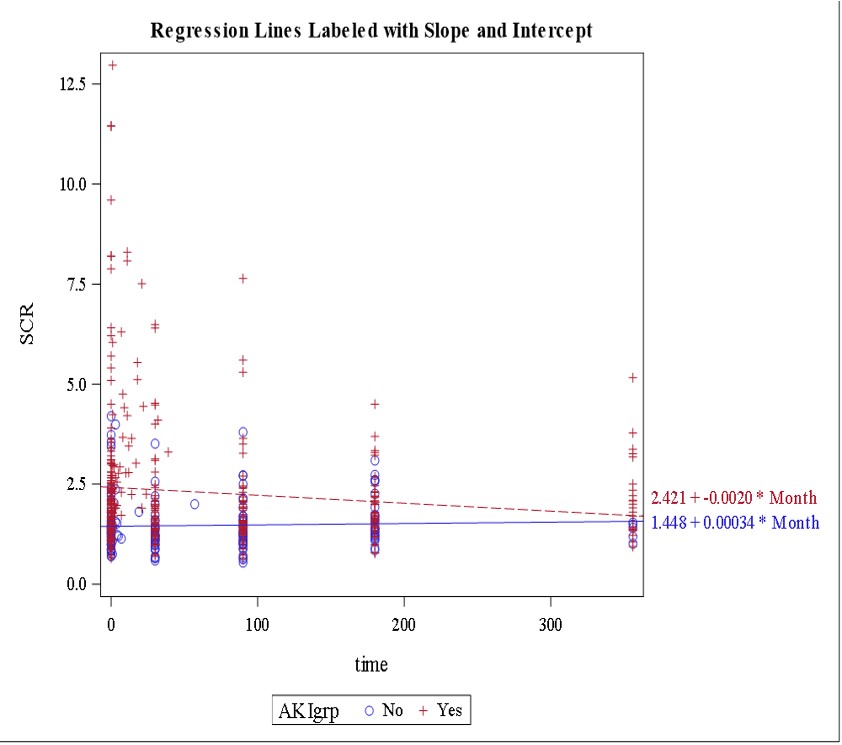
*Results: A total of 149 COVID-19 infected KTRs were hospitalized. Of them, 102 (69%) had AKI with 45 (44.1%) in Stage 1, 9 (8.8%) in Stage 2 and 41 (40.2%) in Stage 3. Thirty-three patients died and 97% of them was in AKI group. Patients in AKI group had median survival time of 1.18 months, compared to more than 8 months in non-AKI group (p=0.002), Figure 1. Regression analysis for Intercept and slope were estimated by AKI groups, showing mild improvement in mean SCR over the 1 year at 2.2 mg/dL from peak SCR of 3.6 mg/dL, lowest eGFR 23.9 (SD 14.39) but didn’t reach pre-AKI baseline in patients with AKI (1.8mg/dL), Figure 2.
*Conclusions: Patients in AKI group had higher mortality most of which was in the early period. There was mild improvement in creatinine over the following 12 months in AKI group but SCR didn’t return to baseline. There with no significant change in slope of creatinine for non-AKI COVID patients.
To cite this abstract in AMA style:
Shrivastava P, Hofmann RM, Norman SP, Granger D, Khoury N, Prashar R, Crombez C, Patel A, Nagai S, Lu M, Samaniego M. One-Year Outcomes in Kidney Transplant Recipients with Acute Kidney Injury and COVID-19 [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/one-year-outcomes-in-kidney-transplant-recipients-with-acute-kidney-injury-and-covid-19/. Accessed February 27, 2026.« Back to 2022 American Transplant Congress