Non-Medical Factors Predict Receipt and Type of Kidney Transplant in Veterans
K. Kendall, X. Li, C.-C. Chang, J. Pleis, E. Croswell, M. Dew, G. Switzer, A. Langone, A. Mittal-Henkle, S. Saha, M. Ramkumar, J. Adams-Flohr, C. Thomas, L. Myaskovsky.
VA Kidney Transplant Centers: IA, OR, PA, TN, Iowa City, Portland, Pittsburgh, Nashville.
Meeting: 2018 American Transplant Congress
Abstract number: 228
Keywords: African-American, Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Psychosocial - 2
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: Room 210
Background: African Americans, Hispanic Americans and other minorities have a higher incidence of end-stage kidney disease but lower rates of both deceased and living donor kidney transplant (DDKT and LDKT) compared to whites. Disparities exist in Veteran's Affairs (VA) and non-VA transplant centers after adjusting for medical factors. We assessed whether race disparities would persist in receipt of kidney transplant (KT) and type of KT received (living or deceased) after adjusting for non-medical factors, including cultural, psychosocial, and knowledge factors (see figure). Methods: We conducted a multicenter longitudinal cohort study of 611 Veterans undergoing initial evaluation for KT at 4 National VA KT Centers from 2010 to 2014. Participants completed an interview shortly after their KT evaluation, and were subsequently tracked via their medical records to document if KT occurred. We used multivariable Fine-Gray proportional subdistribution hazards models for data with competing risks to estimate the rates of receiving a DDKT, a LDKT, or any other type of outcome (i.e., death, withdrawal from wait-list, or still awaiting KT) and the medical and non-medical factors associated with them. Results: Outcomes and predictors can be seen in Figure 1. 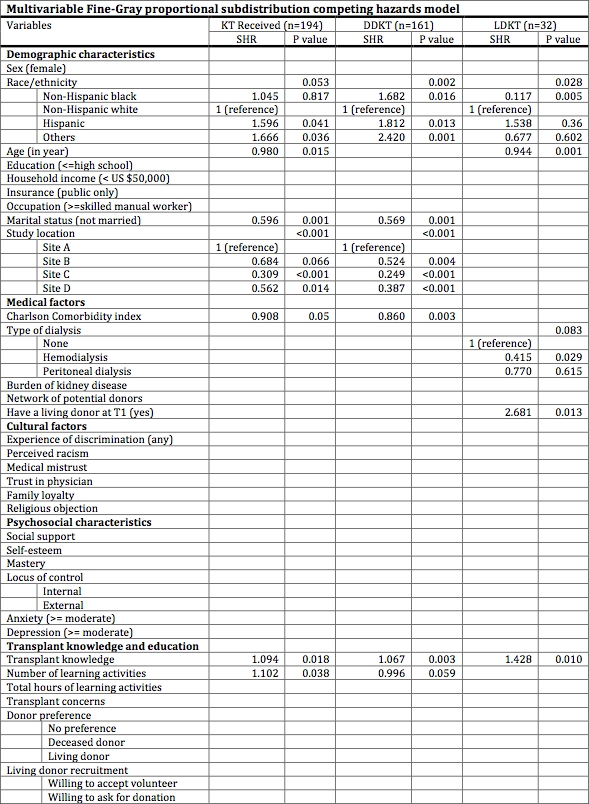 We only included values for the significant predictors from the multivariable models. We used blank spaces to indicate predictors that were not significant. Conclusions: Even though race and several medical factors persisted in predicting transplant outcomes, we found that non-medical factors contributed as well (i.e., age, marital status, having a live donor, transplant knowledge, & learning activities). Our results also indicate that the VA National Transplant System does not exhibit the same pattern of racial disparities in receipt of KT as has been found in other non-VA transplant centers. We also identified important risk factors for receipt of KT among Veterans. VA transplant centers can use these risk factors to identify patients who may be in need of more support to ensure they receive a transplant.
We only included values for the significant predictors from the multivariable models. We used blank spaces to indicate predictors that were not significant. Conclusions: Even though race and several medical factors persisted in predicting transplant outcomes, we found that non-medical factors contributed as well (i.e., age, marital status, having a live donor, transplant knowledge, & learning activities). Our results also indicate that the VA National Transplant System does not exhibit the same pattern of racial disparities in receipt of KT as has been found in other non-VA transplant centers. We also identified important risk factors for receipt of KT among Veterans. VA transplant centers can use these risk factors to identify patients who may be in need of more support to ensure they receive a transplant.
CITATION INFORMATION: Kendall K., Li X., Chang C.-C., Pleis J., Croswell E., Dew M., Switzer G., Langone A., Mittal-Henkle A., Saha S., Ramkumar M., Adams-Flohr J., Thomas C., Myaskovsky L. Non-Medical Factors Predict Receipt and Type of Kidney Transplant in Veterans Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Kendall K, Li X, Chang C-C, Pleis J, Croswell E, Dew M, Switzer G, Langone A, Mittal-Henkle A, Saha S, Ramkumar M, Adams-Flohr J, Thomas C, Myaskovsky L. Non-Medical Factors Predict Receipt and Type of Kidney Transplant in Veterans [abstract]. https://atcmeetingabstracts.com/abstract/non-medical-factors-predict-receipt-and-type-of-kidney-transplant-in-veterans/. Accessed February 19, 2026.« Back to 2018 American Transplant Congress
