No Kidney after Liver Left Behind: An Analysis of the Organ Procurement and Transplantation Network “Safety Net” Policy
Surgery, University of Cincinnati, Cincinnati, OH
Meeting: 2020 American Transplant Congress
Abstract number: 263
Keywords: Allocation, Kidney/liver transplantation, Renal failure, Waiting lists
Session Information
Session Name: Kidney Issues in Liver Transplantation
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:27pm-4:39pm
Presentation Time: 4:27pm-4:39pm
Location: Virtual
*Purpose: Liver transplant (LT) recipients who develop persistent renal dysfunction face increased morbidity and mortality. These patients may be eligible for prioritization on the kidney transplant (KT) waitlist based on the Organ Procurement and Transplantation Network (OPTN) “safety net” policy implemented on August 10, 2017. In this study, we evaluated utilization of KT, as well as waitlist and post-transplant outcomes, of LT recipients with renal dysfunction before and after the implementation of this policy.
*Methods: The United Network for Organ Sharing database from January 2015 to March 2019 was used to evaluate LT recipients who were subsequently placed on the KT waitlist between 60 to 365 days after LT. Characteristics and outcomes of patients on the KT waitlist and the subset who received KT were compared between time periods prior to and after August 10, 2017.
*Results: 119 patients were included in the analysis. The number of LT patients placed on the kidney waitlist increased from 34 before to 85 after the policy. Those who were waitlisted pre- and post-policy had similar demographics and etiology of kidney disease (all p>0.05), but pre-policy patients were more likely to be on dialysis (82.4% vs. 63.5%, p=0.045). Patient and liver graft survival were similar for waitlisted patients before and after the policy (p>0.05 for both).
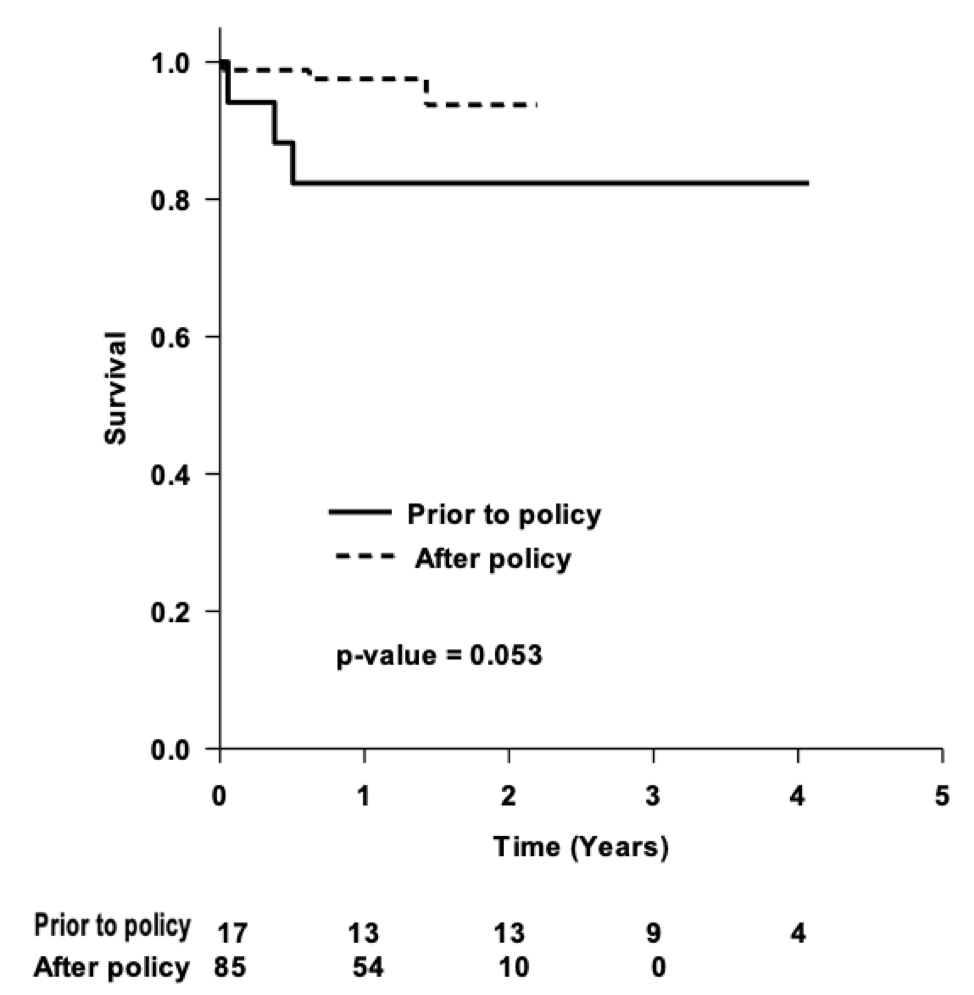
The number of KT in these patients increased from 17 before to 85 after the policy. Those receiving KT after the policy more commonly underwent deceased donor KT (100% vs. 64.7%, p<0.01), received local organs (91.8% vs. 70.6%, p=0.03), and trended towards a shorter time on the waitlist (47 [17-123] vs. 84 [37-226] days, p=0.05). The pre- and post-policy cohorts had similar (all p>0.05) KDPI (0.43 [0.27-0.69] vs. 0.42 [0.28-0.58]), delayed graft function (11.8% vs 14.3%), LOS (5 [4-6] vs. 4 [3-6]), in-hospital mortality (0 in both), and 30-day mortality (0 in both). Patient survival was similar between the pre- and post-policy cohorts, with 1-year survival rates of 93.8% vs. 98.7%, respectively (p>0.05). Kidney graft survival was similar between cohorts (p>0.05). The post-policy cohort showed a trend towards improved liver graft survival (Figure 1, p=0.05).
*Conclusions: This study, for the first time, confirms that the OPTN “safety net” policy, as designed, is effective in increasing the number of LT recipients with renal dysfunction who undergo successful KT with excellent short-term results. Further follow-up will determine if this policy leads to improved long-term survival in LT recipients with renal dysfunction.
To cite this abstract in AMA style:
Lee TC, Wima K, Morris MC, Kassam A, Shah SA, Quillin R. No Kidney after Liver Left Behind: An Analysis of the Organ Procurement and Transplantation Network “Safety Net” Policy [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/no-kidney-after-liver-left-behind-an-analysis-of-the-organ-procurement-and-transplantation-network-safety-net-policy/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress