Moving Beyond the Waitlist in Measurement of Access in Kidney Transplantation
University of British Columbia, Vancouver, BC, Canada
Meeting: 2022 American Transplant Congress
Abstract number: 508
Keywords: Kidney transplantation, Public policy, Survival, Waiting lists
Topic: Clinical Science » Kidney » 50 - Health Equity and Access
Session Information
Session Name: Health Equity and Access II
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 5:30pm-5:40pm
Presentation Time: 5:30pm-5:40pm
Location: Hynes Ballroom C
*Purpose: Studies limited to waitlist candidates have suggested better access to kidney transplantation and fewer disparities in acesss since the new kidney allocation system (KAS) in December 2014. We sought to determine transplant access among all kidney failure patients without contraindications to transplantation.
*Methods: We studied incident kidney failure patients aged 18 to 80 years in the United States Renal Data System who initiated chronic dialysis or were placed on the transplant waiting list before the initiation of dialysis between 1-Jan-2010 & 31-Dec-2017. Patients with a history of tobacco use, heart failure, peripheral vascular disease, cancer, alcohol abuse, atherosclerotic heart disease, chronic obstructive pulmonary disease, or body mass index >38 kg/m2 or <16kg/m2 were excluded. Patients were followed until waitlisting or 3 years post dialysis initiation for the outcome of access to transplantation defined by placement on the transplant waiting list, an administrative requirement prior to any living or deceased kidney transplant in the U.S. Patients were grouped by estimated post-transplant survival (EPTS) score calculated at start of dialysis or first waitlisting. Pre-emptively waitlisted patents were assigned a follow-up time of 0 days. The association of EPTS with access to transplantation, accounting for the competing risk of death, was determined in a multivariable survival analysis (Fine and Gray method). The analysis adjusted for differences in sex, primary kidney disease, race, income by zip code, and timing of study entry (pre or post the new KAS). Whether access to transplantation in Black patients changed after the implemention of the new KAS was determined with the use of an interaction term.
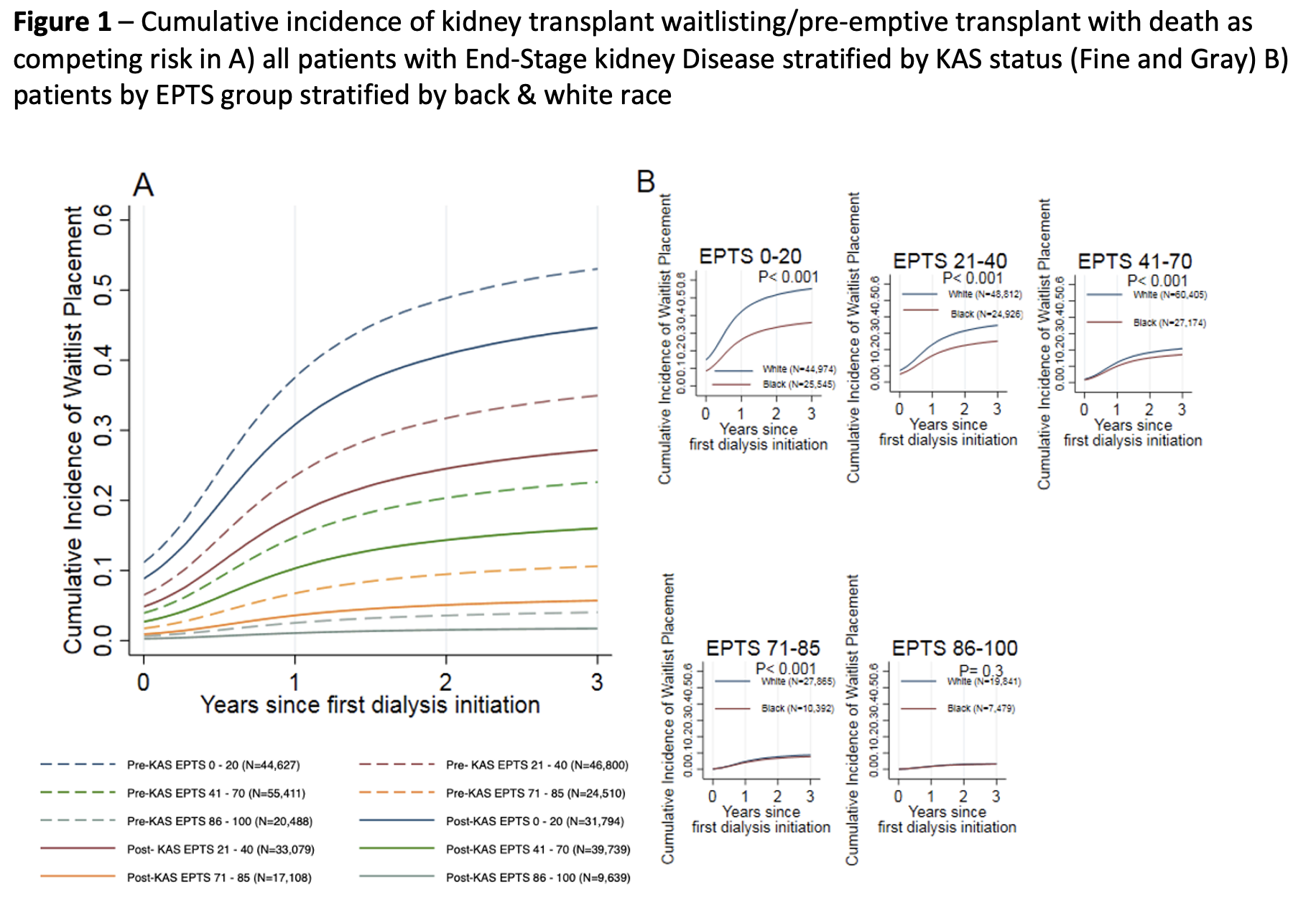
*Results: Among the 323,195 eligible patients, access to transplantation was related to EPTS and was lower post KAS compared to pre KAS in all EPTS groups, Figure 1A. Black patients had lower access compared to White patients especially in patients with favourable EPTS, Figure 1B. In a multivariable analysis, access to transplantation was lower post-KAS (HR 0.74 95% CI 0.72 – 0.75) compared pre-KAS. Black patients had lower access compared to White patients (HR 0.65 95% CI 0.64 – 0.67). Access for Black patients did not improve after the new KAS (HR 0.99 95% CI 0.96 – 1.02 for interaction of race x KAS era).
*Conclusions: In contrast to studies limited to waitlist candidates, access to transplantation and disparities in access to transplantation have not improved post implementation of the new KAS when all incident kidney failure patients without identified contraindications to transplantation are evaluated.
To cite this abstract in AMA style:
McMichael LC, Chang DT, Kadatz M, Gill J. Moving Beyond the Waitlist in Measurement of Access in Kidney Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/moving-beyond-the-waitlist-in-measurement-of-access-in-kidney-transplantation/. Accessed February 21, 2026.« Back to 2022 American Transplant Congress