Missing Self Increases the Incidence of Microvascular Inflammation after Kidney Transplantation
1Microbiology, Immunology and Transplantation, KU Leuven, Leuven, Belgium, 2Histocompatibility and Immunogenetics Laboratory, Red Cross-Flanders, Mechelen, Belgium, 3Imaging and Pathology, KU Leuven, Leuven, Belgium, 4INSERM U1111, Université Claude Bernard Lyon I, Lyon, France
Meeting: 2020 American Transplant Congress
Abstract number: 19
Keywords: Antibodies, Kidney transplantation, Natural killer cells, Rejection
Session Information
Session Name: Kidney Acute Antibody Mediated Rejection
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:15pm-3:27pm
Presentation Time: 3:15pm-3:27pm
Location: Virtual
*Purpose: Anti-HLA donor-specific antibodies (HLA-DSA) are often absent in serum of kidney allograft recipients with biopsies demonstrating microvascular inflammation (MVI), the histological hallmark of antibody-mediated rejection. Recent animal and in vitro studies have shown that endothelial cell damage can be induced independently from antibodies through missing self (MS), defined as the inability of donor endothelial cells to provide HLA I-mediated signals to inhibitory KIR receptors on recipient natural killer (NK) cells. The importance of missing self-associated NK cell activity in kidney allograft histology and outcome remains unclear.
*Methods: In a single-center cohort study of 924 kidney transplantations between 2004 and 2013, high-resolution donor and recipient HLA typing, and recipient KIR genotyping were performed. Missing self was defined as absence of Bw4, C1 or C2 donor genotype, in presence of a corresponding educating inhibitory KIR gene in the recipient (KIR3DL1, KIR2DL2/3 or KIR2DL1, respectively).
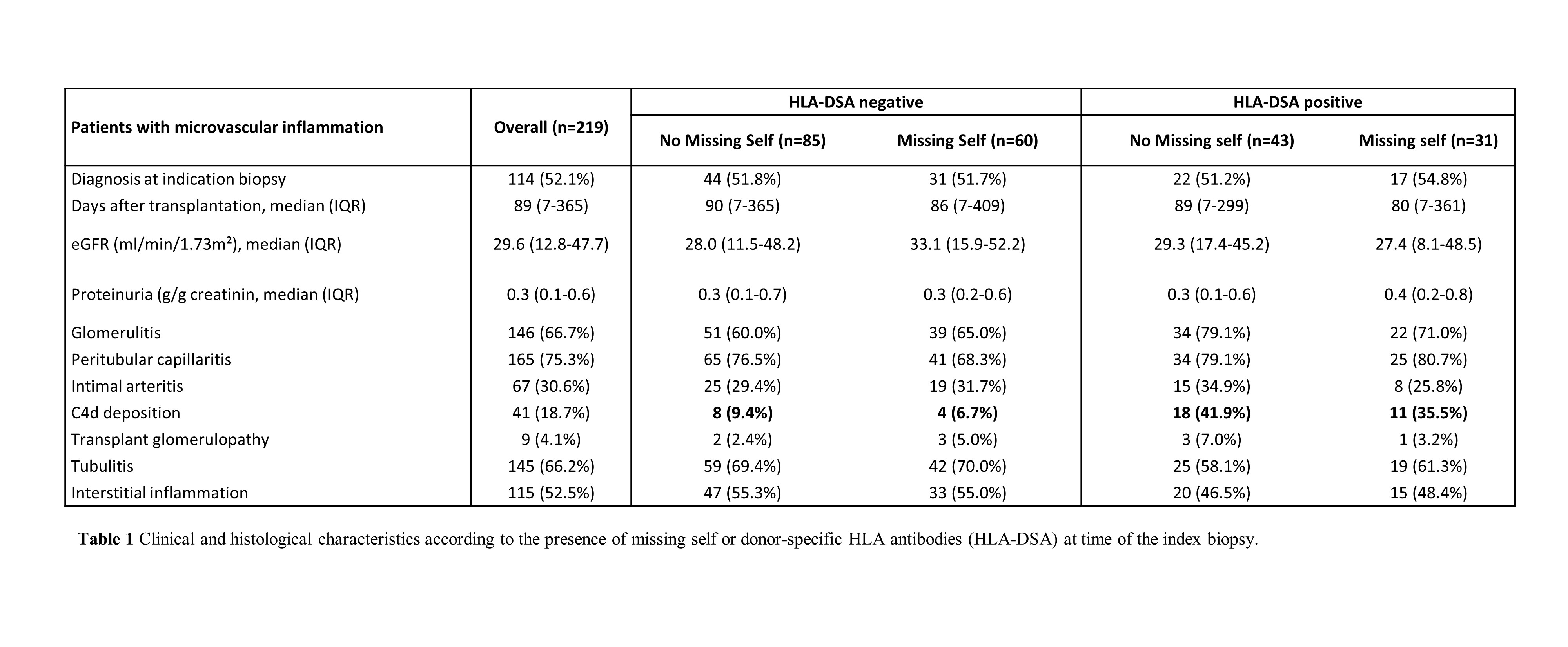
*Results: We identified missing self in 329/924 (35.6%) donor-recipient pairs. Missing self associated with a higher incidence of MVI after transplantation (HR 1.37, 95% CI 1.06-1.78, P=0.018). In multivariate analysis, increased missing self (range 0-3) increased risk of MVI (HR per unit increase 1.28, 1.08-1.53), independent from HLA-DSA. There was no association between missing self and borderline changes or T-cell mediated rejection. MS+DSA- MVI was characterized by less C4d deposition compared to MS-DSA+ MVI (6.7% vs 41.9%, P<0.001), without other histological differences. Nevertheless, missing self did not significantly increase risk for allograft failure after MVI diagnosis (HR 1.58, 0.92-2.71, P=0.10), in contrast to HLA-DSA (HR 2.07, 1.19-3.58, P=0.010).
*Conclusions: Kidney transplantation with missing self, a trigger for NK cell activation, significantly increases risk of MVI, independent of HLA-DSA. The clinicopathological phenotype of HLA-DSA-negative MVI associated with missing self is similar to HLA-DSA-positive MVI, although allograft survival is better. Including missing self in the evaluation of the donor-recipient mismatch improves our understanding of HLA-DSA-negative MVI and could be relevant for pre-transplant risk assessment.
To cite this abstract in AMA style:
Callemeyn J, Senev A, Coemans M, Lerut E, Sprangers B, Kuypers D, Koenig A, Thaunat O, Emonds M, Naesens M. Missing Self Increases the Incidence of Microvascular Inflammation after Kidney Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/missing-self-increases-the-incidence-of-microvascular-inflammation-after-kidney-transplantation/. Accessed February 27, 2026.« Back to 2020 American Transplant Congress