Microvascular Inflammation without Antibody Mediated Rejection in Renal Transplantation
Thomas E. Starzl Transplantation Institute, UPMC, Pittsburgh, PA
Meeting: 2022 American Transplant Congress
Abstract number: 209
Keywords: Antibodies, Kidney, Rejection
Topic: Clinical Science » Kidney » 34 - Kidney: Acute Cellular Rejection
Session Information
Session Name: Kidney: Acute Cellular Rejection
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:50pm-4:00pm
Presentation Time: 3:50pm-4:00pm
Location: Hynes Ballroom A
*Purpose: Microvascular inflammation (MVI) defined by glomerulitis (g) and peritubular capillaritis (ptc) is a hallmark of ABMR in renal transplantation. The prevalence and significance of MVI in patients without ABMR is less understood.
*Methods: Here, we analyzed MVI in the 1st post-transplant year, its relationship to DSA, and its clinical significance in a large cohort of patients without ABMR. Along with any for-cause biopsy (fcBx), patients underwent 2 protocol biopsies (pBx, 3 & 12mos). Bx were categorized as early (0-4mos) or late (5-12mos). Serum was screened for DSA at 0, 1, 3, 6, 9 & 12mos post-transplant.
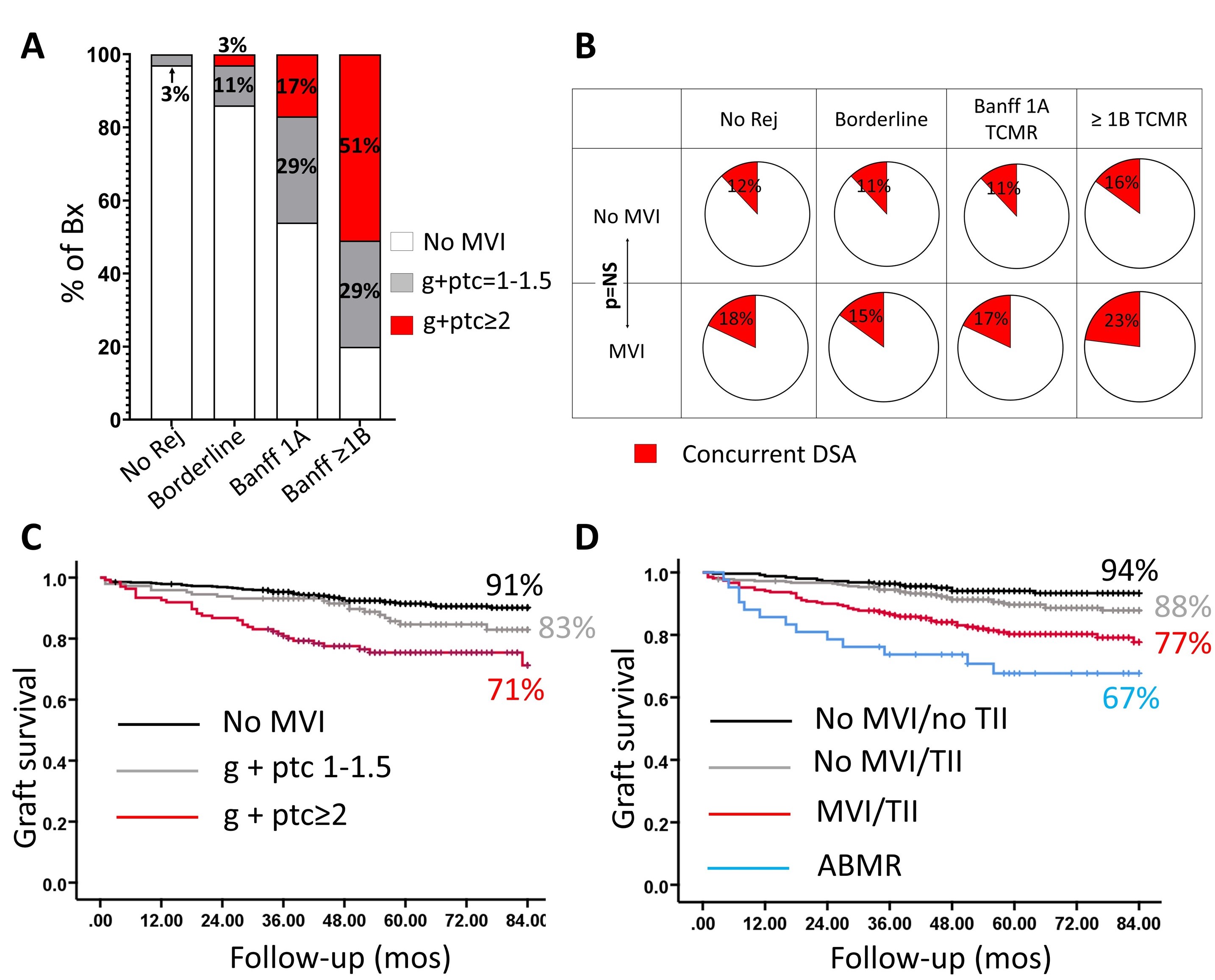
*Results: MVI Prevalence: 956/1187 patients transplanted between 2013-18 underwent 1950 Bx (67% protocol, 33% for-cause). Of these Bx, 64 had either ABMR or GN and were excluded. MVI was noted in 23% (g+ptc score 1-1.5 in 13% & ≥2 in 10%) of the remaining 1887 Bx with greater prevalence in fcBx (fcBx 14% vs. pBx 7%) and late Bx (late Bx 29% vs. early Bx 17%). Of note, the MVI prevalence and its severity increased with increasing grades of tubulointerstitial inflammation (TII) (Fig 1A, no Rejection vs. Borderline vs. 1A TCMR vs. >1B TCMR, all p<0.05). Moreover, 65% of patients with allograft infections (pyelonephritis & BKVN) had MVI. MVI & DSA: DSA was detected concurrently in 12% of all the 1887 Bx without ABMR. Although, MVI was associated with concurrent DSA detection in these Bx (OR 1.8, 95% CI 1.3-2.5, p<0.,001), ~60% of the biopsies never had DSA (concurrent/historic or future). Furthermore, in biopsies stratified by the grade of TCMR, there was no significant difference in concurrent DSA detection between patients with and without MVI (Fig.1B). Outcomes: MVI in patients without ABMR was associated with decreased 7yr-graft survival (Fig 1C, no MVI vs. ‘g’+’ptc’ 1-1.5, p<0.05, no MVI vs. 'g'+'ptc' >2, p<0.001). The combination of MVI and TII was associated with worse graft survival when compared to either no inflammation or TII alone (Fig1D, no TII/no MVI vs. MVI/TII, p<0.001; TII/no MVI vs. TII/MVI, p=0.001). Further, in a select sub-group of patients with allograft infection, MVI was associated with a trend towards decreased graft survival compared to no MVI (76% vs. 88%). Finally, in a Cox multivariable model, MVI was associated with poor graft survival independent of potential confounders including DSA (HR 2.5, 95% CI 1.6-3.4, p<0.001).
*Conclusions: MVI is common even in the absence of ABMR or DSA and is a marker for the severity of allograft inflammation and subsequent poor clinical outcomes.
To cite this abstract in AMA style:
Saba JBou, Chowdhury R, Mehta R, Abou-Daya KI, Hariharan S, Cherukuri A. Microvascular Inflammation without Antibody Mediated Rejection in Renal Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/microvascular-inflammation-without-antibody-mediated-rejection-in-renal-transplantation/. Accessed February 17, 2026.« Back to 2022 American Transplant Congress