Medication Non-Adherence (MNA) Mitigation Practices and Health Care Professional (HCP) Perceptions at U.S. Transplant Centers
S. J. Patel1, J. L. Descourouez2, B. Hofmeyer3, C. A. Moore4, D. Nguyen5, E. Graviss5, D. J. Taber6
1Veloxis Pharmaceuticals, Cary, NC, 2UW Health, Madison, WI, 3Mercy Hospital, Iowa City, IA, 4UPMC Presbyterian Hospital, Pittsburgh, PA, 5Houston Methodist, Houston, TX, 6MUSC, Charleston, SC
Meeting: 2020 American Transplant Congress
Abstract number: B-099
Keywords: Immunosuppression, Kidney, Psychosocial
Session Information
Session Name: Poster Session B: Kidney Psychosocial
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Extensive literature exists on risk factors and mitigating strategies for MNA, however information on MNA management within U.S. transplant centers is scarce. This survey aimed to gather current practices at transplant centers and perceptions of HCPs regarding MNA at their centers.
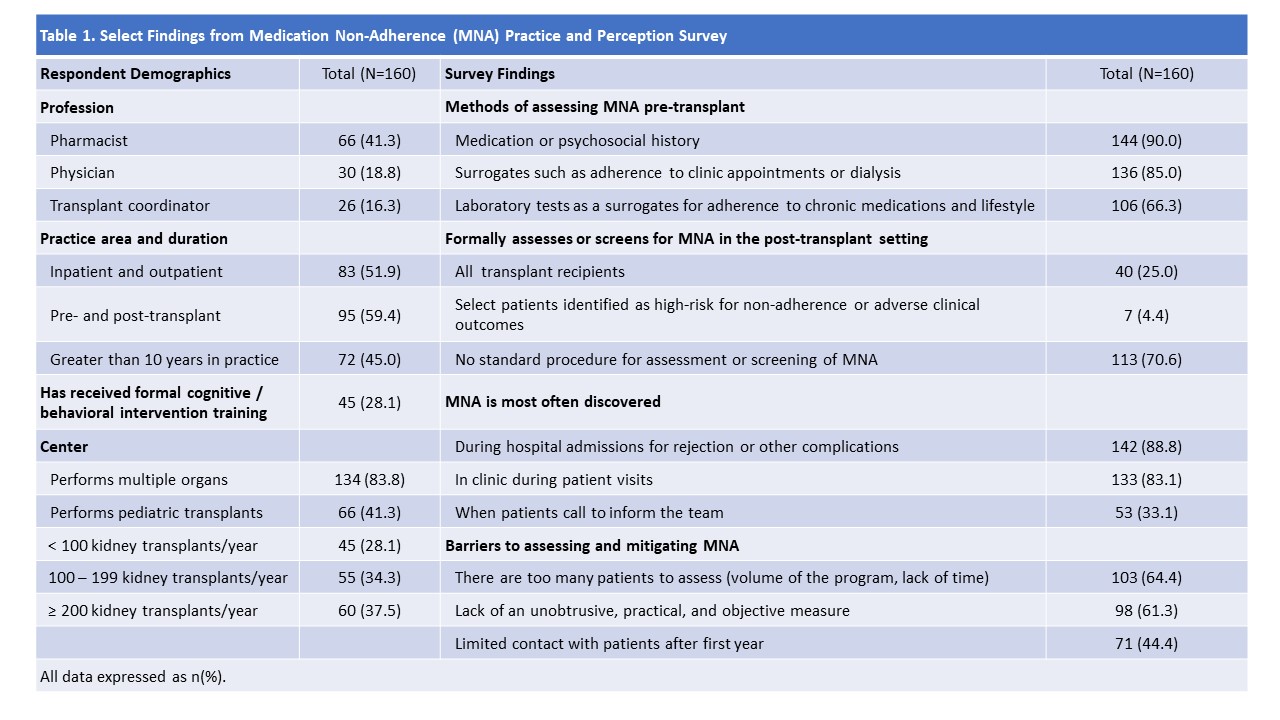
*Methods: We conducted a 29-question survey of HCPs involved in the management of adult kidney transplant recipients at U.S. centers.
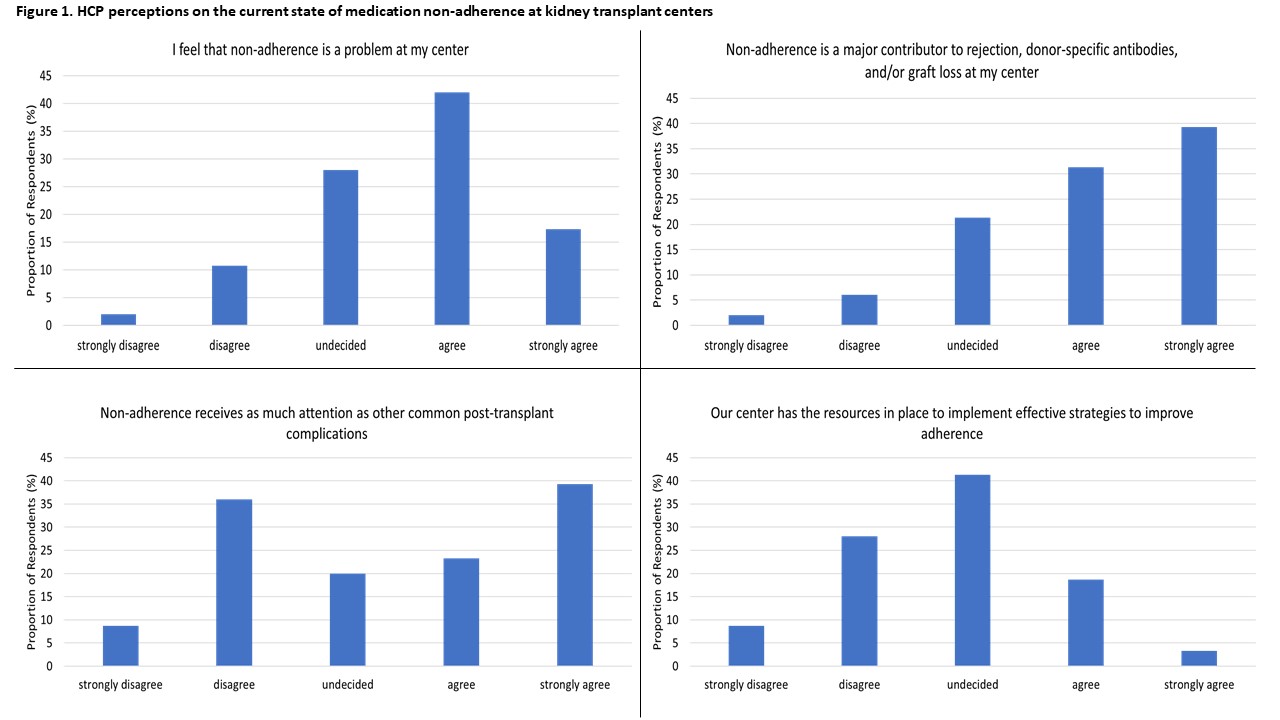
*Results: Responses from 160 HCPs from 81 centers were included (demographics in Table 1). Most respondents agreed that MNA was a problem at their center (59%) and a major contributor to rejection and graft loss (71%), though fewer felt that MNA received as much attention as other post-transplant complications (35%), or that their center had resources in place to implement strategies to mitigate MNA (22%; Figure 1). Most participants acknowledged not having any standard procedure for assessing MNA post-transplant (71%). Of those who did report having a standard procedure, MNA assessments declined over time (first post-transplant month: 92%; 1 – 3 years post-transplant: 40%; >3 years: 36%) and the most common methods of capturing MNA were immunosuppressant level deviations (85%) and prompting patients to report MNA (72%). Only 17 respondents reported use of an adherence questionnaire. Most cases of MNA were reported as being discovered during admissions for rejection or complications (89%). Common barriers to use of MNA mitigation strategies included lack of time/resources (64%) and lack of an unobtrusive, practical measure (61%). Most respondents identified the most ideal characteristics of MNA mitigation strategies as having little-to-no obstruction of workflow (76%) and being evidenced-based (69%).
*Conclusions: While HCPs feel that MNA is a major problem at their centers, the use of protocols or systematic processes aimed at identifying and mitigating MNA is rare. Opportunities exist to address MNA at transplant centers, and feasible strategies which adapt to HCP workflow are urgently needed.
To cite this abstract in AMA style:
Patel SJ, Descourouez JL, Hofmeyer B, Moore CA, Nguyen D, Graviss E, Taber DJ. Medication Non-Adherence (MNA) Mitigation Practices and Health Care Professional (HCP) Perceptions at U.S. Transplant Centers [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/medication-non-adherence-mna-mitigation-practices-and-health-care-professional-hcp-perceptions-at-u-s-transplant-centers/. Accessed February 25, 2026.« Back to 2020 American Transplant Congress