Living Donor Conversion Rates as a Quality Measure for Kidney Program Efficiency for Both New Referrals and Existing Listed Candidates
1U of Cincinnati, Cincinnati, OH, 2UC Health, Cincinnati, OH, 3U of Arkansas, Little Rock, AR
Meeting: 2019 American Transplant Congress
Abstract number: 130
Keywords: Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Living Donor: Quality and Selection
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:42pm-5:54pm
Presentation Time: 5:42pm-5:54pm
Location: Ballroom A
*Purpose: Arguably the most important achievement for renal failure patients is identification of a living donor (LD)and transplantation with a LD kidney. Given these considerations LD conversion rate (LDCR) has been previously reported as a potential quality metric for kidney transplant programs. Herein, we expand upon this concept with increased specificity by calculating LDCR for recently referred kidney transplant candidates (viz, by determining LDCR for new wait listings (ie, waiting times < 1 year) and also for existing waitlisted patients (ie, waiting times > 1 year). The UNOS requirement that all kidney transplant recipients be wait listed prior to transplantation has greatly increased the integrity of data used to calculate these rates. Herein we examine these new concepts.
*Methods: OPTN/SRTR data was used for all calculations. Formulae used to calculate New Listing LDCR (NL-LDCR) was #LD kidney transplants with < 1 year waiting time in most recent year/# new wait listings in the same year for each kidney transplant program. Existing listing LDCR (EL-LDCR) was calculated using #LD with >1 year waiting time/#wait listed patients at the beginning of the year.
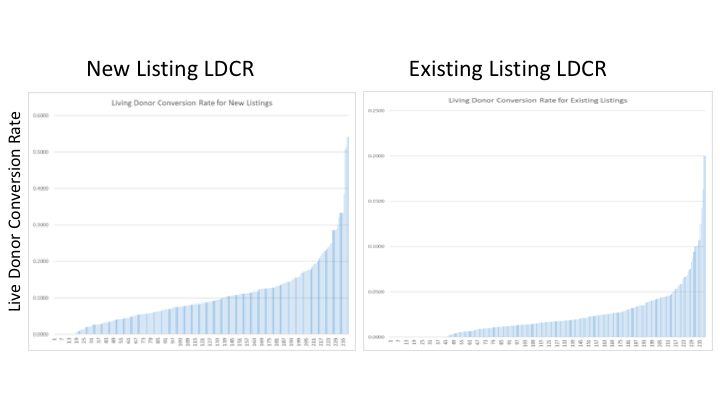
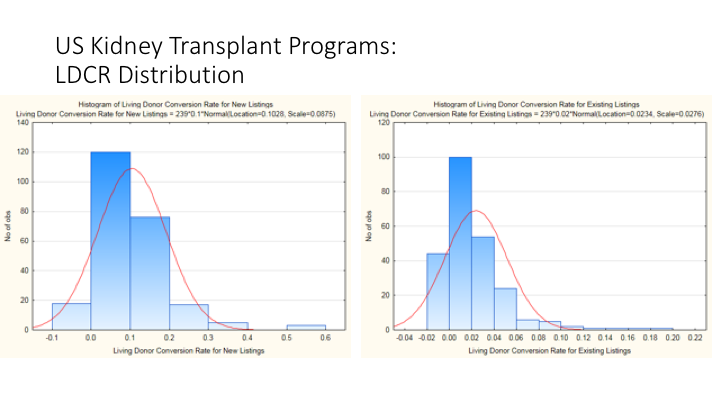
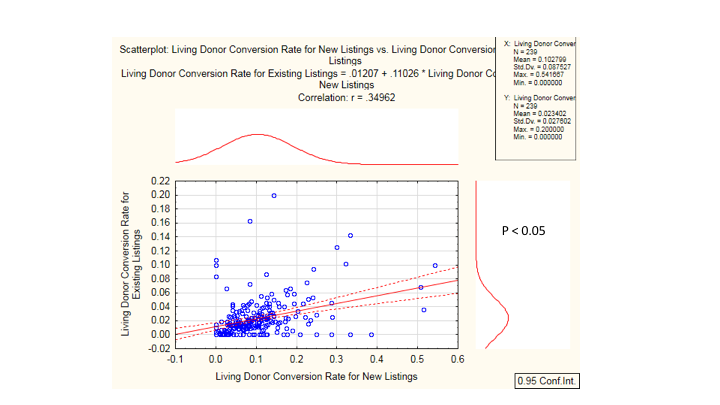
*Results: Figure 1 presents data for over 260 US kidney transplant programs for NL-LDCR and EL-LDCR. Marked variability in NL-LDCR was observed amongst programs varying from 0% to almost 60%. EL-LDCR demonstrated a 1-2 log lower rate of LDCR (between 0 -20%), and with a lesser degree of heterogeneity amongst transplant programs. Finally, regression analysis examining the relationship between NL-LDCR and EL-LDCR for individual programs demonstrated a relatively low correlation rate (r=0.34) that was significant however,, indicating heterogeneity in processes for achieving LD transplantation involve differing processes.
*Conclusions: Kidney transplant program efficiency at achieving LD transplantation can now be measured by two approaches- NL-LDCR and EL-LDCR that show significant heterogeneity amongst US programs, indicating substantial room for growth in many programs. Importantly, achieving LD transplantation in a newly referred patient is a different process that achieving LD transplantation in a chronically wait listed patient, and these data indicate that processes should be developed and widely adopted that help address the low LDCR in this population.
To cite this abstract in AMA style:
Woodle E, Siemers C, Woodle B, King C, Alloway R, Tremblay S. Living Donor Conversion Rates as a Quality Measure for Kidney Program Efficiency for Both New Referrals and Existing Listed Candidates [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/living-donor-conversion-rates-as-a-quality-measure-for-kidney-program-efficiency-for-both-new-referrals-and-existing-listed-candidates/. Accessed February 22, 2026.« Back to 2019 American Transplant Congress