Liver Outcomes and Equity (LOEq) Index: Neighborhood-Level Social Determinants of Health and Waitlist Disparities for Adult Liver Transplantation
University of Southern California, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 390
Keywords: Mortality, Risk factors, Waiting lists
Topic: Clinical Science » Liver » 55 - Liver: Recipient Selection
Session Information
Session Time: 8:25am-9:30am
 Presentation Time: 9:15am-9:30am
Presentation Time: 9:15am-9:30am
Location: Hynes Veterans Auditorium
*Purpose: Impact of neighborhood-level social determinants of health (SDOH) among adult liver transplant (LT) candidates is largely unknown. We constructed a novel index (LOEq) to characterize area-based SDOH specific to the population with liver disease in the United States (US) and examined outcome of waitlist (WL) mortality.
*Methods: The LOEq index was derived from 16,713 unique ZIP codes (42% of US ZIP codes) of adult waitlisted patients in the Scientific Registry of Transplant Recipients database from 6/18/2013-5/18/2018. We used a structured and iterative principal component analysis method to reduce 38 American Community Survey (2014-2018) variables across five SDOH domains to 13 for inclusion in the LOEq index. For analysis, status 1, re-transplants, and MELD exception applications were excluded to focus on the cirrhotic population. Primary predictor was LOEq index quintiles (Q1=lowest to Q5=highest SDOH). Outcome was WL mortality examined in multivariate competing risk regression models with transplant wait region and demographic/clinical factors.
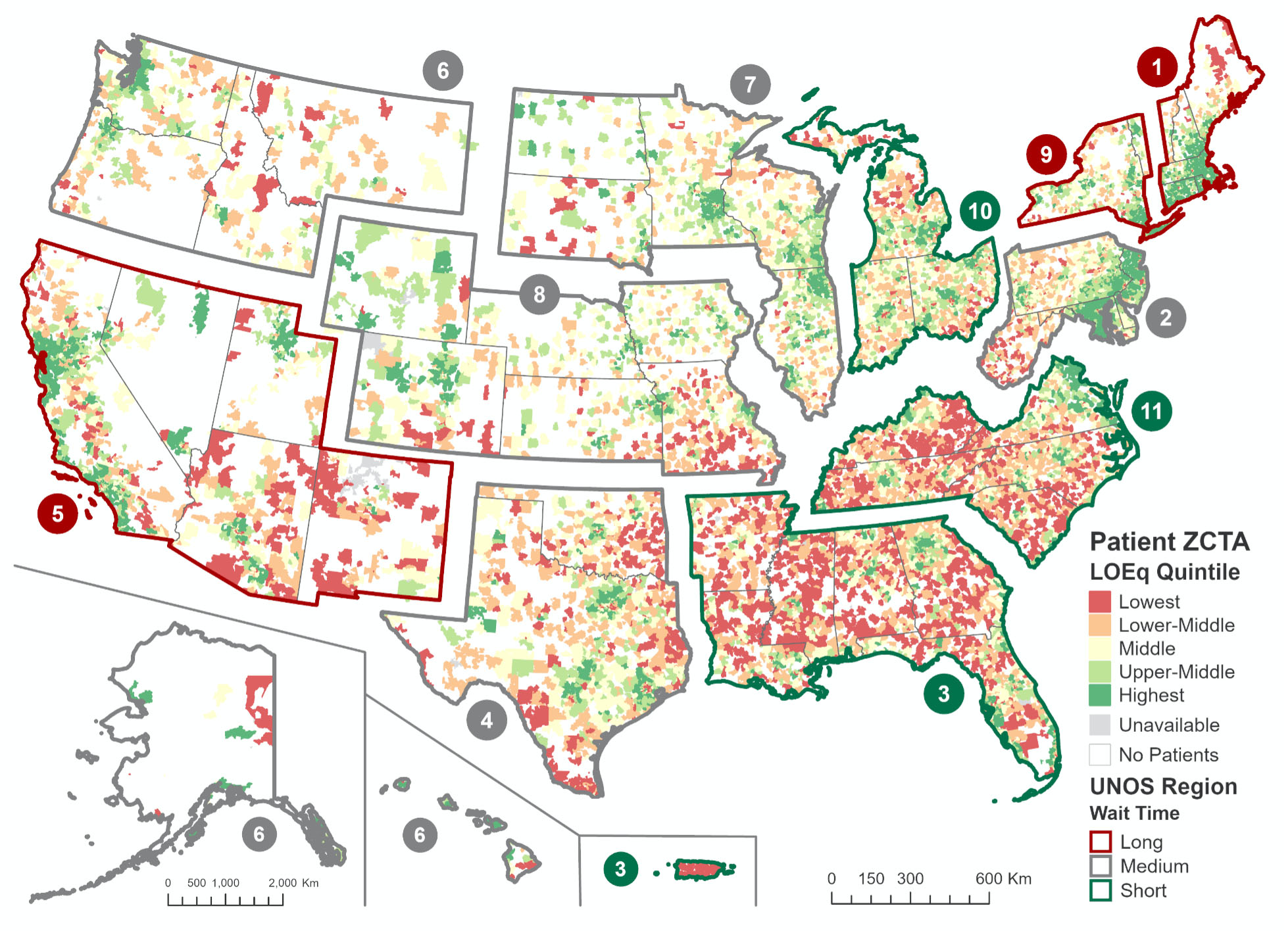
*Results: Distribution of the 39,422 adult LT candidates across the US favored neighborhoods with higher SDOH, with double the number in Q5 vs Q1 (39.9% vs 13.9%). Lower LOEq quintiles had higher proportion Hispanic or Black, public insurance, hepatitis C etiology, diabetes, and obesity. The 3-year cumulative incidence of WL mortality was higher in Q1 (23.2%, 21.9-24.4%) vs Q5 (20.8%, 20.0-21.6%). There was a marked geographic concentration of lower LOEq quintiles in short wait time transplant regions (Figure): 49% of Q1 vs 18% of Q5. With bivariate adjustment for wait region, LOEq Q1-4 were associated with increased WL mortality vs Q5 (all p<0.01), with Q1 patients incurring 29% excess deaths compared to Q5 (HR 1.29, 95% CI 1.20-1.39). In the full model, similar results were found, with 24% excess deaths (HR 1.24, 1.15-1.34) in Q1 followed by 15%, 12% and 13% for Q2, Q3, and Q4, respectively (all p<0.01). There was a non-significant interaction between LOEq and alcohol etiology: higher WL mortality for Q1 vs Q5 for those with alcohol (HR 1.33) vs other etiologies (HR 1.16; p-interaction=0.09).
*Conclusions: A neighborhood-level disparity in access to LT exists with candidates disproportionately residing in high SDOH areas. Despite higher concentration in short wait time regions, lower neighborhood SDOH was associated with increased WL mortality. The liver disease-specific LOEq index is a novel tool to identify vulnerable US neighborhoods for interventions to promote LT equity.
To cite this abstract in AMA style:
Zhou K, Kuo LS, Thompson LK, Dodge JL, Cockburn MG, Terrault N. Liver Outcomes and Equity (LOEq) Index: Neighborhood-Level Social Determinants of Health and Waitlist Disparities for Adult Liver Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/liver-outcomes-and-equity-loeq-index-neighborhood-level-social-determinants-of-health-and-waitlist-disparities-for-adult-liver-transplantation/. Accessed March 6, 2026.« Back to 2022 American Transplant Congress