Late Rejection in Pediatric Heart Transplantation: The Importance of Medical Adherence
Division of Pediatric Cardiology, Columbia University, New York, NY.
Meeting: 2015 American Transplant Congress
Abstract number: D254
Keywords: Heart transplant patients, Pediatric, Rejection
Session Information
Session Name: Poster Session D: "The Tell-Tale Heart": Allograft Rejection and Post-Transplant Monitoring
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
While the incidence of early rejection (<1 yr post-transplant) after pediatric heart transplant (HT) has decreased, late rejection (> 1 yr post-transplant) remains a constant risk associated with adverse graft outcomes. Why the risk of late rejection has not declined in the same fashion as that of early rejection remains unknown.
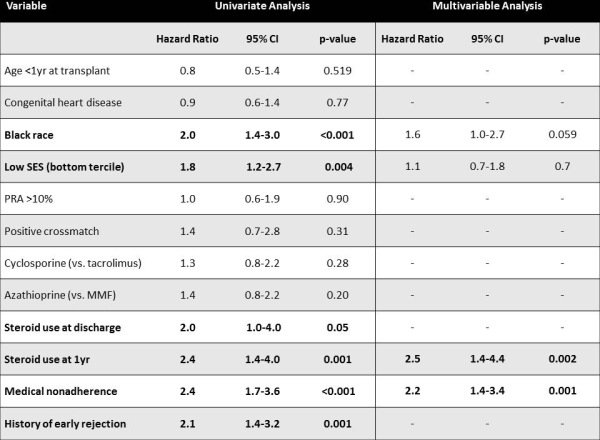
We performed a retrospective review of all pediatric HT recipients at our institution between 1/1/93-6/30/13. Demographic and clinical data, including recipient socioeconomic status (household income in the lowest tercile), medical adherence, immunosuppression regimens and early rejection were analyzed using Cox Proportional Hazard modeling of risk factors for late rejection.
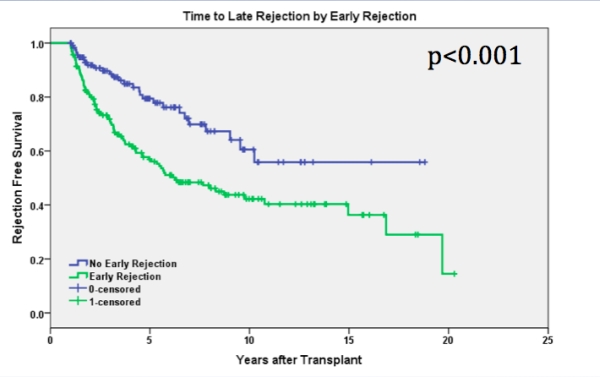
Of 338 patients, 183 (54%) experienced at least one episode of early rejection, while only 109 experienced late rejection; with a median follow-up time of 5.3yrs (IQR 1.9-9.6yrs). The median time from HT to late rejection was 3yrs (IQR 1.6-5.1yrs) with an average age at first late rejection of 14yrs (IQR 7.2-18.3yrs). Time to late rejection was significantly shorter (Figure 1) and the median age at late rejection was younger (11.8 vs. 15.5yrs, p= 0.04) for those with a history of early rejection. Univariate and multivariable analysis is shown in Figure 2, with only medical nonadherence and steroid use at 1 yr remaining as independent predictors. Late rejection was associated with graft failure (45% vs. 13%, p<0.001) and coronary vasculopathy (43% vs. 20%, p<0.001)
In conclusion, in pediatric HT recipients, controlling for race and socioeconomic status, medical nonadherence is one of the most important risk factors for late graft rejection. These findings suggest that therapies aimed at adherence is required to improve the incidence of late graft rejection and long-term graft survival.
To cite this abstract in AMA style:
Letica A, Zuckerman W, Addonizio L, McAllister J, Lee T, Richmond M. Late Rejection in Pediatric Heart Transplantation: The Importance of Medical Adherence [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/late-rejection-in-pediatric-heart-transplantation-the-importance-of-medical-adherence/. Accessed February 17, 2026.« Back to 2015 American Transplant Congress
