Late Acute Rejection Increases Risk Of Graft Failure In Ldlt Recipients: Data From The A2all Cohort
H. J. Braun, J. L. Dodge, J. D. Grab, S. M. Syed, G. R. Roll, C. E. Freise, J. P. Roberts, N. L. Ascher
University of California, San Francisco, San Francisco, CA
Meeting: 2019 American Transplant Congress
Abstract number: 43
Keywords: Living-related liver donors
Session Information
Session Name: Concurrent Session: Liver: Immunosuppression and Rejection
Session Type: Concurrent Session
Date: Sunday, June 2, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:06pm-3:18pm
Presentation Time: 3:06pm-3:18pm
Location: Room 312
*Purpose: Late acute rejection (LAR) is defined as an initial episode of acute rejection occurring >6 months after transplantation. LAR in liver transplantation (LT) is associated with an increased risk of graft failure and death. The purpose of this study was to examine LAR in recipients of living donor liver transplantation (LDLT) and deceased donor liver transplantation (DDLT) using data from the Adult-to-Adult Living Donor Liver Transplantation Study (A2ALL) cohort to determine the impact of LAR on graft and patient survival.
*Methods: A2ALL recipients who underwent LDLT or DDLT between April 1998 and January 2014 were included. We compared recipients with biopsy proven early acute rejection (EAR), LAR, and no acute rejection using Kruskal-Wallis and Chi-squared tests; logistic regression assessed factors associated with late versus early acute rejection. Post-LT graft and patient survival were estimated using Kaplan-Meier methods and differences assessed by Cox proportional hazards regression modeling rejection as a time-varying covariate.
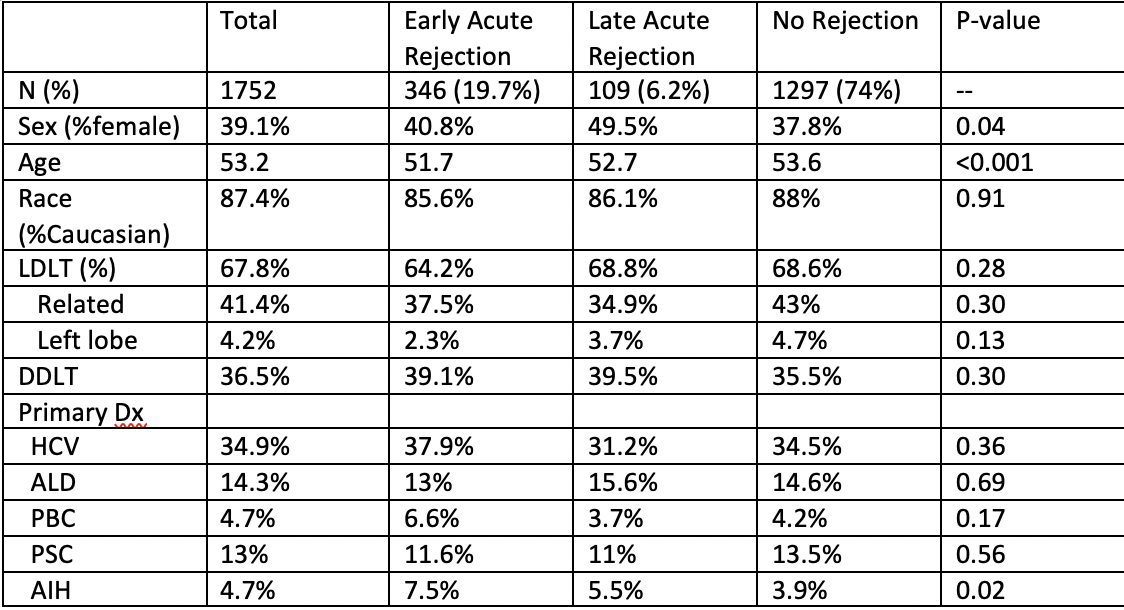
*Results: 1752 patients were included, 1187 were LDLT recipients and 565 were DDLT recipients. A total of 346 (19.7%) had EAR and 109 (6.2%) developed LAR (75 (6.3%) and 34 (6.0%) LDLT and DDLT recipients, respectively, (p=0.28)). Demographic data is summarized in Figure 1. In univariate logistic regression, no factors were identified that predicted LAR versus EAR. Among subjects with LAR, 5- and 10-year post-LT graft survival was 82.9% (95% CI 73.8-89.0) and 57.4% (95% CI 44.7-68.2), respectively, and patient survival was 84.7% (95% CI 75.8-90.5) and 59.7% (95% CI 46.7-70.5), respectively. LAR subjects receiving LDLT vs DDLT had similar 10-year post-LT graft (54.9% vs 62.2%, p=0.47) and patient (58.0% vs 62.9%, p=0.42) survival. Using multivariable Cox regression adjusting for age, race, diagnosis, and LDLT, risk of graft loss was significantly higher for patients with LAR compared to no rejection (HR 1.79, 95% CI 1.25-2.57, p=0.001) but not death (HR 0.96, 95% CI 0.66-1.39, p=0.84). Patients who received a graft from a related donor were at higher risk for graft loss if they developed LAR (HR 1.72, 95% CI 1.17-2.54, p=0.006). Subjects with LDLT were not at increased risk of graft loss or death (HR=0.98, 95% CI 0.83-1.17, p=0.84; HR=0.91, 95% CI 0.76-1.09, p=0.30). The impact of LAR on graft and patient survival was similar for LDLT and DDLT recipients (interaction p=0.49 and p=0.45).
*Conclusions: Approximately 6.2% of patients in the A2ALL cohort developed LAR. LAR was associated with increased risk of graft loss.
To cite this abstract in AMA style:
Braun HJ, Dodge JL, Grab JD, Syed SM, Roll GR, Freise CE, Roberts JP, Ascher NL. Late Acute Rejection Increases Risk Of Graft Failure In Ldlt Recipients: Data From The A2all Cohort [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/late-acute-rejection-increases-risk-of-graft-failure-in-ldlt-recipients-data-from-the-a2all-cohort/. Accessed March 1, 2026.« Back to 2019 American Transplant Congress