Kidney Transplant Outcomes by Living Donor (LD) Relationship
Scientific Registry of Transplant Recipients (SRTR), Minneapolis Medical Research Foundation, Minneapolis, MN
Department of Surgery, University of Minnesota, Minneapolis, MN
Meeting: 2013 American Transplant Congress
Abstract number: B923
From 2007 to 2011, the proportion of LDs from paired kidney donor (PKD) programs tripled (3.5%-10.8%) and from non-directed donors (NDD) doubled (1.3%-2.6%). As these donor sources grow, it is important to understand the impact of living donor relationship on outcomes.
Methods: Using SRTR standard analysis files, we examined 3-year all-cause graft survival and patient survival among 23,421 LD kidney transplant recipients, 2007-2010, by 7 LD relationships. Follow-up was censored at 10/31/11; identical twin donors (N=40) were excluded. Survival was estimated with Kaplan-Meier methods. To account for confounders, we also considered Cox proportional hazard models adjusted for donor and recipient age, PRA, donation year, and recipient diabetes status. LD relationship was as reported to OPTN.
Results: Unadjusted graft survival ranged from 93% among recipients of a sibling’s kidney to 89% among NDD recipients. After adjustment, graft failure (GF) risk was 21% lower (HR: 0.821, P=0.0036) for sibling kidneys than for the reference group, unrelated donors. Outcomes for all other relationships, including PKD and NDD, were similar to unrelated donor outcomes.
Unadjusted patient survival ranged from 99% among recipients of a parent’s kidney to 94% for recipients of their child’s kidney. After adjustment, risk of death was 25% lower for recipients of a sibling’s kidney than for recipients with unrelated donors (HR: 0.799, P=0.0272). Outcomes for all other groups, including PKD and NDD, were similar to unrelated donor outcomes.
Figure 1: Hazard ratios for risk of GF and death by donor relationship.
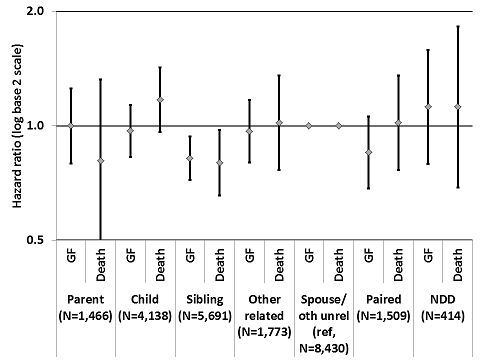
Conclusions: While sibling donors provide improved 3-year graft and patient outcomes compared with unrelated donors, all other donor relationships, including PKD and NDD, provide similarly good graft and patient outcomes.
To cite this abstract in AMA style:
Skeans M, Snyder J, Matas A. Kidney Transplant Outcomes by Living Donor (LD) Relationship [abstract]. Am J Transplant. 2013; 13 (suppl 5). https://atcmeetingabstracts.com/abstract/kidney-transplant-outcomes-by-living-donor-ld-relationship/. Accessed February 26, 2026.« Back to 2013 American Transplant Congress
