Introduction of Direct Acting Antivirals for HCV: Fewer Kidney Discards but a Long Way to Go
T. Alhamad,1 R. Thakkar,1 D. Brennan,2 J. Lappin,3 B. Kaplan,3 A. Malone,1 V. Hicks,1 J. Wellen,1 K. Lentine.4
1Washington University in St. Louis, St. Louis
2Johns Hopkins University, Baltimore
3Baylor Scott and White, Temple
4Saint Louis University, St. Louis.
Meeting: 2018 American Transplant Congress
Abstract number: 40
Keywords: Donation, Hepatitis C
Session Information
Session Name: Concurrent Session: Kidney Infectious - Viral Hepatitis
Session Type: Concurrent Session
Date: Sunday, June 3, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Room 4C-4
Organ shortage remains a great challenge facing the field of kidney transplantation. Donor hepatitis C virus positivity (DHCV+) is one of the highest ranking factors contributing to the kidney donor profile index (KDPI), increasing the KDPI by approximately 20% pushing it to levels high enough to preclude renal allograft acceptance by many centers. Since 2014, Direct Acting Antiviral (DAA) therapy has resulted in 95% sustained viral response rate deemed a “cure”. Little is known if the availability and efficacy of DAA has lowered organ discard rates of DHCV+ kidneys.
We examined OPTN data on the disposition of renal allografts (2000 to 12/2016). Associations of DHCV+ with discard (adjusted odds ratio, 95% LCL aOR 95% UCL) were quantified by multivariate Logistic regression including adjustment for other donor factors.
Overall, 5,683 DHCV+ and 123,520 DHCV- renal allografts were in the study period. The overall kidney discard rate at any KDPI for DHCV+ organs was 55% between 2005 and 2014, declined to 40% in 2015 and 2016 compared to ≤ 21% in DHCV-. With KDPI>85%, the discard rate for DHCV+ vs. DHCV- kidneys was 56.1% vs. 49.0%, while for KDPI 51-85%, the discard rate with DHCV+ vs. DHCV- was 49.2% and 22.2%. DHCV+ kidneys were associated with 3.7-times higher risk for discard (aOR 3.433.663.91) compared to DHCV-. Among the KDPI factors, significant risk factors for discard (P<0.05) were older age, obesity, diabetes, hypertension, donation after cardiac death, and cause of death secondary to stroke, anoxia, or CNS tumor (compared to head trauma). 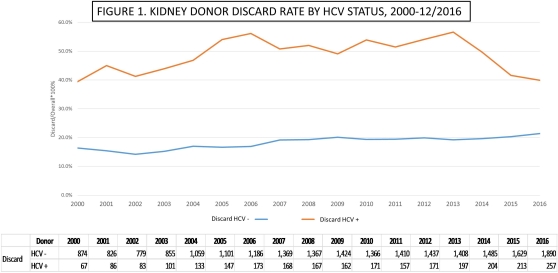
In the last two years, DHCV+ kidneys have a decreasing but consistently higher discard rate compared to DHCV- kidneys despite the availability of DAA. Among the KDPI factors, DHCV+ status carries the highest weight for discard. Further studies are needed to maximize the appropriate utilization of DHCV+ kidneys in the current era where options for successful treatments do exist.
CITATION INFORMATION: Alhamad T., Thakkar R., Brennan D., Lappin J., Kaplan B., Malone A., Hicks V., Wellen J., Lentine K. Introduction of Direct Acting Antivirals for HCV: Fewer Kidney Discards but a Long Way to Go Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Alhamad T, Thakkar R, Brennan D, Lappin J, Kaplan B, Malone A, Hicks V, Wellen J, Lentine K. Introduction of Direct Acting Antivirals for HCV: Fewer Kidney Discards but a Long Way to Go [abstract]. https://atcmeetingabstracts.com/abstract/introduction-of-direct-acting-antivirals-for-hcv-fewer-kidney-discards-but-a-long-way-to-go/. Accessed February 19, 2026.« Back to 2018 American Transplant Congress
