Intensive Monitoring and Early Treatment for Urinary Infection in Renal Transplant Recipients Reduces Readmission and Sepsis
A. Patel, S. Desai, B. R. Schleich, M. Wynd, T. Carrea, Y. Yushkov, S. Geatrakas, N. White, R. Luongo, R. Sosnicki, V. Wadhera, D. Serur, M. J. Goldstein
Organ Transplant, Hackensack University Medical Center, Hackensack, NJ
Meeting: 2021 American Transplant Congress
Abstract number: 793
Keywords: Infection, Kidney, Urinalysis
Topic: Clinical Science » Infectious Disease » Kidney Infectious Non-Polyoma & Non-Viral Hepatitis
Session Information
Session Name: Kidney Infectious Non-Polyoma & Non-Viral Hepatitis
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Urinary tract infection (UTI) is a common renal transplant (RT) complication that is observed in up to 60-70% of RT recipients and may affect allograft function and long-term survival. A retrospective review identified an opportunity for reduction in the adverse events related to post-RT UTI. We hypothesized that implementation of an early detection and treatment program would reduce the incidence of readmission and complications from UTI after RT.
*Methods: An intensive, prospective UTI monitoring and treatment performance improvement plan (PIP) was established in April 2018. A retrospective cohort study was conducted comparing patient outcomes after PIP with cases before implementation. We defined bacteriuria as having 25,000 to 100,000 and UTI having more than 100,000 bacteria present on urine culture. Urinalysis and urine culture were sent on all RT recipients weekly for 1-month post-RT Recipients at higher risk (recurrent history of UTI before RT, urinary retention history and congenital or acquired urogenital abnormalities ) for UTI were monitored for 3 months.
All symptomatic patients within 3 months and all asymptomatic patients within 1 month of RT with bacteriuria on uncontaminated urinalysis were treated empirically. High risk, asymptomatic patients within 3 months of RT with bacteriuria on uncontaminated urinalysis were treated empirically.
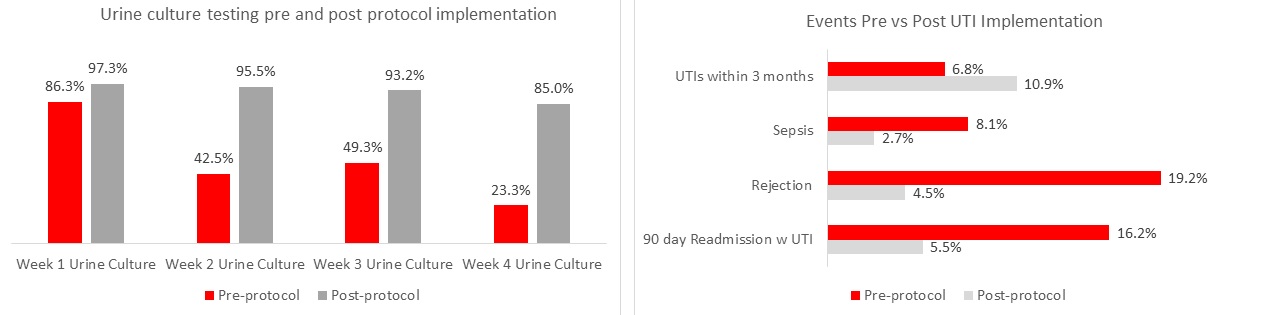
*Results: A retrospective data analysis comparing RT case controls (N=73) and post PIP implementation (N=220) was conducted. Figure 1 shows that the prevalence of urine testing was much higher post protocol implementation. Despite a higher 3-month UTI rate most likely detected through more screening, post-RT outcomes were significantly (p<0.05) improved after PIP implementation for 90-day readmissions with UTI, diagnosis of sepsis, and rejection (Figure 2).
*Conclusions: The 11% UTI rate observed within 3 months resulting from this PIP is one among the lowest observed. The reported high incidence of UTI and adverse outcomes related to this complication can be mitigated through intensive monitoring, detection, and a lower threshold for early treatment. While protocol testing identified a slightly higher incidence of UTI relative to case controls, as expected, there was a significant reduction in the severity of disease requiring a readmission for UTI or sepsis. We did not identify adverse effects of early antibiotic intervention for symptomatic or asymptomatic bacteriuria.
To cite this abstract in AMA style:
Patel A, Desai S, Schleich BR, Wynd M, Carrea T, Yushkov Y, Geatrakas S, White N, Luongo R, Sosnicki R, Wadhera V, Serur D, Goldstein MJ. Intensive Monitoring and Early Treatment for Urinary Infection in Renal Transplant Recipients Reduces Readmission and Sepsis [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/intensive-monitoring-and-early-treatment-for-urinary-infection-in-renal-transplant-recipients-reduces-readmission-and-sepsis/. Accessed March 4, 2026.« Back to 2021 American Transplant Congress