Induction Immunosuppression Does Not Worsen Tumor Recurrence After Liver Transplantation for T2 Hepatocellular Carcinoma and May Allow for Decreased Mortality
1Gastroenterology, University of Pennsylvania, Philadelphia, PA, 2Biostatistics, University of Pennsylvania, Philadelphia, PA
Meeting: 2022 American Transplant Congress
Abstract number: 34
Keywords: Hepatocellular carcinoma, Immunosuppression, Survival, Tumor recurrence
Topic: Clinical Science » Liver » 56 - Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Hepatocellular Carcinoma and Other Malignancies
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:50pm-4:00pm
Presentation Time: 3:50pm-4:00pm
Location: Hynes Room 312
*Purpose: Prior studies have suggested that induction therapy leads to worse outcomes after liver transplantation (LT) for hepatocellular carcinoma (HCC). This study evaluated the impact of induction immunosuppression (IS) on post-LT survival and tumor recurrence among patients with T2 HCC nationally.
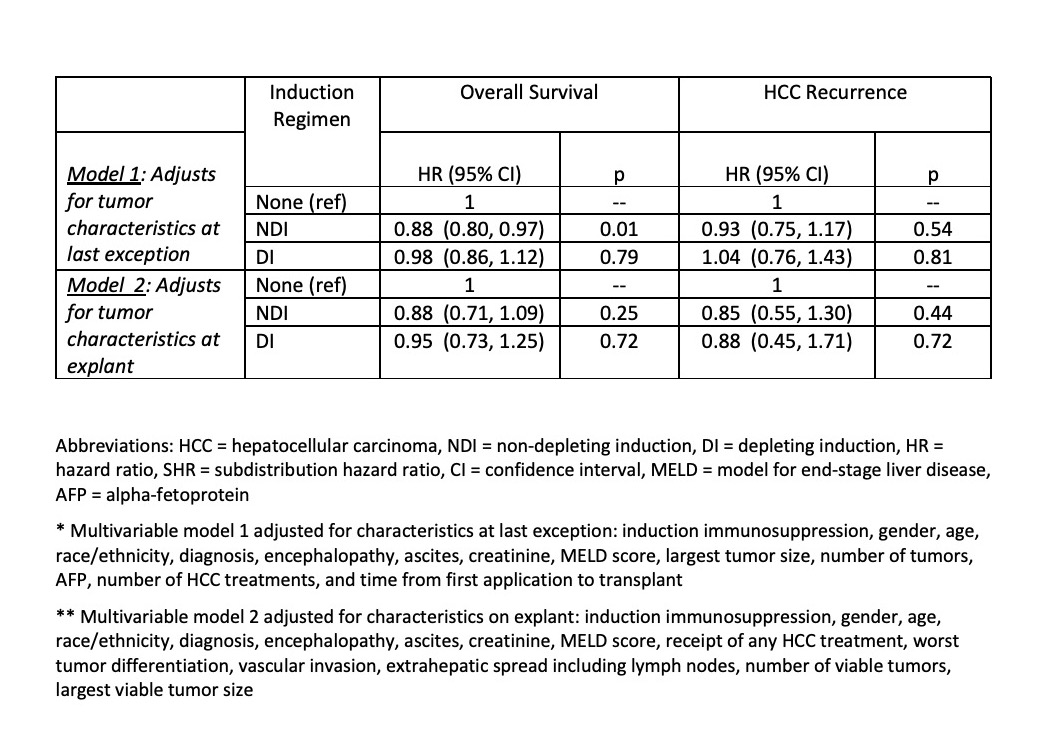
*Methods: A retrospective cohort of adult LT alone recipients with T2 HCC between 2/27/2002 and 3/31/2019 was identified in the United Network for Organ Sharing database. Time-to-event analyses evaluated the association of induction therapy (none, non-depleting [NDI], depleting [DI]) with overall survival and HCC recurrence (with death as a competing event). Models were stratified by center to prevent confounding by center in a flexible manner, given marked differences in induction practices. Separate multivariable models adjusted for tumor characteristics on last exception application (simulating what is known at the time of induction decision-making) or on explant (simulating the biologic effect of induction).
*Results: The study cohort included 22,535 LT recipients with T2 HCC, of which 17,688 (78.48%) received no induction, 2,984 (13.24%) NDI, and 1,863 (8.27%) DI. Few differences in patient and tumor characteristics were noted between induction groups. Significant center variability in induction use for HCC patients (median 11.71%, IQR: 2.17-45.94%). At LT hospital discharge, three-drug IS was least frequent for the DI group (17.49% vs 52.24% for NDI vs 64.74% for no induction; p<0.001). In adjusted stratified analyses, NDI was associated with improved overall survival accounting for exception tumor features (adjusted HR=0.88 vs no induction, p=0.01; Table). DI was not associated with survival (all p>0.1; Table). The HCC recurrence rate was 5.05% and was not associated with either NDI or DI (all p>0.1; Table).
*Conclusions: Induction IS was not associated with worse post-LT outcomes in patients transplanted for T2 HCC. Similar to the non-HCC population, a small but significant improvement in overall survival was observed with NDI versus no induction in T2 HCC patients.
To cite this abstract in AMA style:
Durkin C, Bittermann T, Schaubel DE. Induction Immunosuppression Does Not Worsen Tumor Recurrence After Liver Transplantation for T2 Hepatocellular Carcinoma and May Allow for Decreased Mortality [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/induction-immunosuppression-does-not-worsen-tumor-recurrence-after-liver-transplantation-for-t2-hepatocellular-carcinoma-and-may-allow-for-decreased-mortality/. Accessed February 26, 2026.« Back to 2022 American Transplant Congress