Individual and Community-Level Social Determinants of Health in Liver Transplant
1General Surgery, University of California, San Francisco, San Francisco, CA, 2University of California, San Francisco, San Francisco, CA, 3UCSF, San Francisco, CA, 4Kaiser Permanente Northern California, San Francisco, CA, 5UCSF Medical Center, San Francisco, CA
Meeting: 2022 American Transplant Congress
Abstract number: 72
Keywords: Hepatocellular carcinoma, Outcome, Outpatients, Waiting lists
Topic: Clinical Science » Organ Inclusive » 70 - Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Information
Session Name: Disparities to Outcome and Access to Healthcare
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:10pm-4:20pm
Presentation Time: 4:10pm-4:20pm
Location: Hynes Room 311
*Purpose: To investigate the individual and census-level social determinants of health on liver transplant listing.
*Methods: Retrospective review of patients referred to the University of California San Francisco (UCSF) liver transplant center between 2013 – 2015. The primary outcome of interest was referral outcome (list vs deny). Chi-squared analysis was used to compare the distributions of categorical variables between the two referral outcome groups. Socioeconomic trends were captured as geographic variation using neighborhood deprivation index (NDI; Messer et al, 2006), which is composed of measures of socioeconomic status including wealth and income, education, occupation, and housing condition. NDI is ranked 1-5, with 5 being the highest deprivation. Multivariable logistic regression models were built using both individual and census-level social determinants of health, and adjusted for liver-disease factors (HCC, MELD, disease etiology).
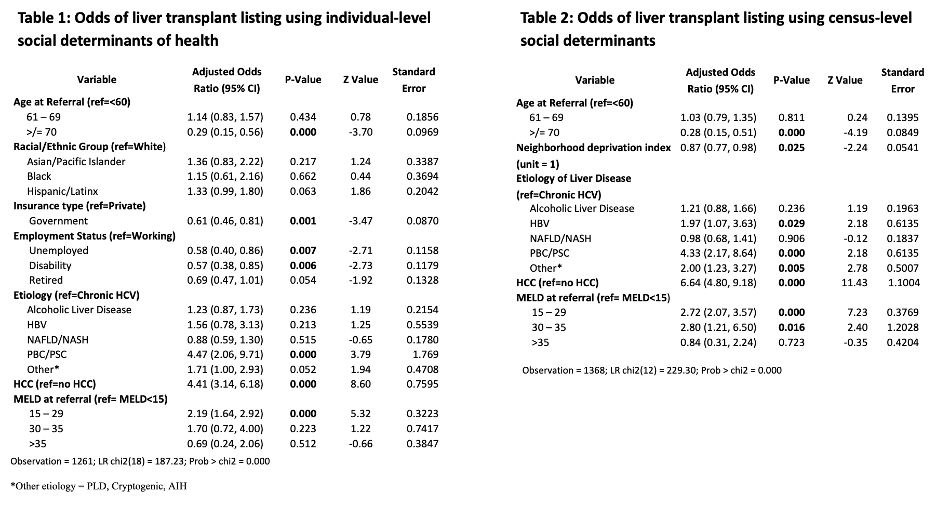
*Results: Out of 1656 adult patients referred, 54% were listed. 51% where White, 67% male, 87% spoke English, 63% had commercial insurance, 35% were employed, and 52% had higher than high school education. In univariate analysis, race/ethnicity, age at referral, insurance, employment, NDI, HCC, disease etiology, and MELD were all significantly associated with referral outcome. Multivariable logistic regression using significant variables from univariate analysis found that older age, government insurance, and unemployed or disability (ref=working) were associated with lower odds of listing. On the other hand, PBC/PBS (ref = HCV), HCC, and MELD 15-29 (ref= MELD <15) were associated with higher odds of listing (Table 1). Multivariable logistic regression using census-level social determinants of health (NDI) found that older age and increase in one unit of NDI had lower odds of listing; in the same model, HBV, PBC/PSC, HCC, and MELD 15-35 all had higher odds of listing (Table 2).
*Conclusions: Individual and community-level social determinants of health are associated with patients not being listed even after adjusting for liver disease specific variables (HCC, MELD, and disease etiology). For each unit of increase in neighborhood deprivation index there was a 23% lower odds of listing, even when adjusting for HCC, MELD, and disease etiology.
To cite this abstract in AMA style:
Yilma M, Cogan R, Mehta N, Neuhaus J, Voelkel J, Light C, Allen I, Hirose R. Individual and Community-Level Social Determinants of Health in Liver Transplant [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/individual-and-community-level-social-determinants-of-health-in-liver-transplant/. Accessed February 19, 2026.« Back to 2022 American Transplant Congress