Incidence, Clinical Correlates and Outcomes of Pulmonary Hypertension after Kidney Transplantation: Analysis of Linked U.S. Registry and Medicare Billing Claims
K. Lentine1, S. Costa2, Y. Caliskan3, D. Levine4, J. Runo5, H. Te6, J. Rangaswami7, D. Dadhania8, D. Axelrod9, M. Schnitzler3, H. Xiao1, B. Kasiske10, J. Snyder10, T. Villines11
1Department of Medicine, Saint Louis Univ, Saint Louis, MO, 2Dartmouth, Lebanon, NH, 3Saint Louis Univ, Saint Louis, MO, 4UT Health, San Antonio, TX, 5Univ of Wisconsin, Madison, WI, 6Univ of Chicago, Chicago, IL, 7Einstein Medical Ctr, Philadelphia, PA, 8Weill Cornell, New York, NY, 9Univ of Iowa, Iowa City, IA, 10SRTR, Minneapolis, MN, 11Univ of Virginia, Charlottesville, VA
Meeting: 2020 American Transplant Congress
Abstract number: B-043
Keywords: Kidney transplantation, Outcome, Pulmonary hypertension, Risk factors
Session Information
Session Name: Poster Session B: Kidney: Cardiovascular and Metabolic Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: To describe the incidence and mortality implications of pulmonary hypertension (P-HTN) in a large, national cohort of US kidney transplant (KTx) recipients.
*Methods: We examined a linkage of Scientific Registry of Transplant Recipients data with Medicare claims to investigate P-HTN diagnoses among Medicare-insured KTx recipients in 2000-2016 (N=59,610). We identified diagnoses of P-HTN based on International Classification of Diseases, Clinical Modification (ICD-CM) diagnostic codes (ICD-CM-9 through October 2015, then ICD-CM-10) on billing claims. Cox regression was used to identify independent correlates of P-HTN (adjusted hazard ratio, 95% LCLaHR 95%UCL), and to examine P-HTN diagnoses as time-dependent mortality predictors, stratified by baseline clinical factors.
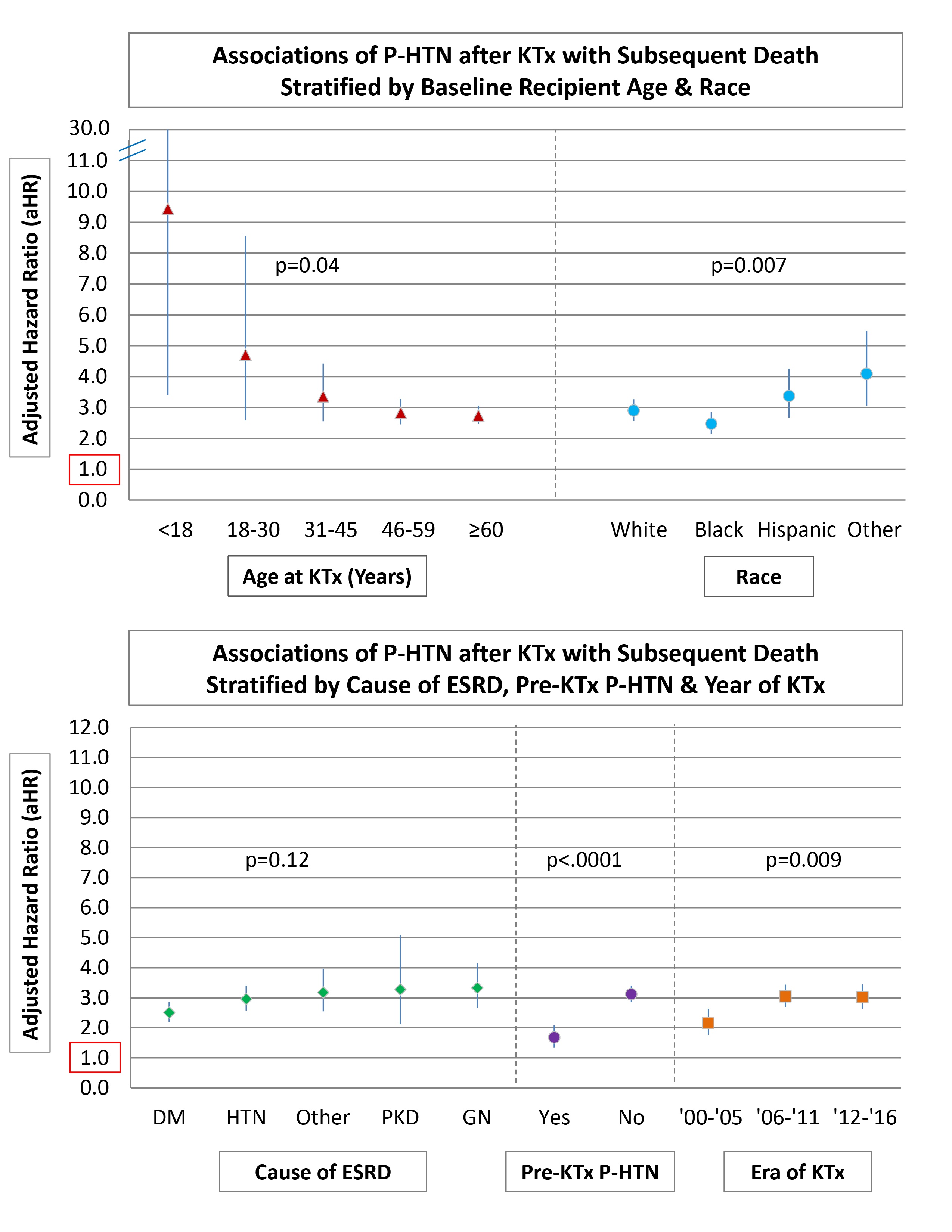
*Results: At 3 years post-KTx, P-HTN was diagnosed in 7.0% of those without P-HTN in the year before KTx, but in 45.8% of those with P-HTN in the year before KTx. Among those without pre-KTx P-HTN, incidence of new onset was higher with baseline factors including older age (aHR for age >60 vs <18-30, 2.382.933.60), obesity (aHR, 1.081.19 1.31), limited baseline functional status (aHR, 1.111.261.44), coronary artery disease (1.21 1.351.51), chronic obstructive lung disease (aHR 1.561.942.41), longer pre-KTx dialysis duration (aHR for >5 yrs vs preemptive, 1.321.48 1.66), dialysis modality (aHR for hemo- vs peritoneal, 1.24 1.42 1.63), and lower organ quality (aHR kidney donor profile index >85 vs 20-25, 1.17 1.30 1.45). P-HTN diagnosis was associated with 2.8-fold increased risk of mortality overall, with relative risk highest in recipients who were younger or of non-white/non-black race, with kidney failure due to glomerulonephritis or polycystic kidney disease, without pretransplant P-HTN, and who underwent transplant more recently (Fig).
*Conclusions: Clinical diagnosis of P-HTN after KTx is correlated with increased risk of subsequent mortality. More work is needed to refine diagnostic and management strategies to improve outcomes in KTx recipients who develop this challenging complication.
To cite this abstract in AMA style:
Lentine K, Costa S, Caliskan Y, Levine D, Runo J, Te H, Rangaswami J, Dadhania D, Axelrod D, Schnitzler M, Xiao H, Kasiske B, Snyder J, Villines T. Incidence, Clinical Correlates and Outcomes of Pulmonary Hypertension after Kidney Transplantation: Analysis of Linked U.S. Registry and Medicare Billing Claims [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/incidence-clinical-correlates-and-outcomes-of-pulmonary-hypertension-after-kidney-transplantation-analysis-of-linked-u-s-registry-and-medicare-billing-claims/. Accessed March 1, 2026.« Back to 2020 American Transplant Congress