Incidence and Risk Factors of Post-Transplant Erythrocytosis in Deceased Donor Kidney Transplantation
S. Alasfar, Y. Jia, I. E. Hall, H. Thiessen Philbrook, S. G. Mansour, M. D. Doshi, S. Mohan, J. S. Bromberg, P. P. Reese, C. Parikh
DDS Consortium, Baltimore, MD
Meeting: 2020 American Transplant Congress
Abstract number: A-054
Keywords: Cadaveric organs, Kidney transplantation, Metabolic complications
Session Information
Session Name: Poster Session A: Kidney: Cardiovascular and Metabolic Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Post-transplant erythroytosis (PTE) is clinically important condition after kidney transplantation (KTx). Previously published literature from single-center studies, demonstrated variable incidence rates between 8-15%. We sought to determine the incidence rate and risk factors of PTE with modern immunosuppression and current transplant practices. We also tested the hypothesis that the risk of PTE is greater with higher-quality kidneys [i.e., lower kidney donor profile index (KDPI)] in deceased-donor KTx
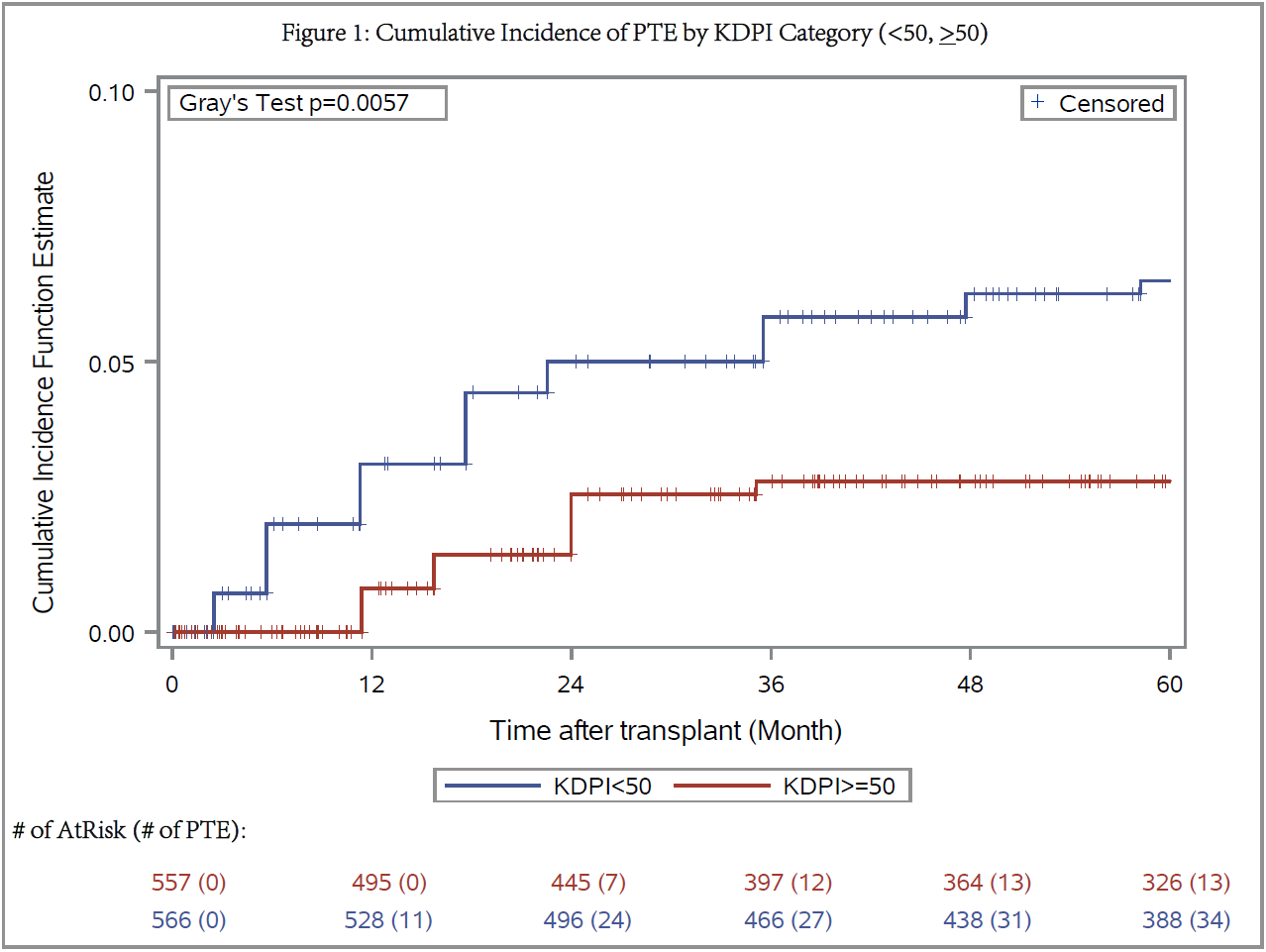
*Methods: We performed detailed chart review for 1137 adult KTx recipients who received deceased-donor KTx from 2010-2013 at 13 centers. PTE was defined as hemoglobin (Hb) >17g/dL in males and >16 g/dL in females. 14 recipients were excluded due to unavailable laboratory data. Descriptive statistics were used to assess PTE risk factors and the relationship between KDPI and PTE. The impact of PTE on graft outcomes was assessed using time-dependent covariate cox models
*Results: PTE was observed in 47 (4.1%) recipients over a median follow-up of 60 months (IQR 36-60). Median time to development of PTE was 18 months (IQR 18-24). Compared to recipients without PTE, those with PTE were younger [mean age 46±13 (yr±SD) vs 54±13, p<0.001), had lower mean BMI [26.6 vs 28.4 kg/m2, p=0.018], received kidneys from younger donors [mean age 35±13 vs 42±15, p=0.003], and had lower mean cold ischemia time [14.8 vs 16.4 hr, p=0.04]. Those with PTE were less likely to receive kidneys from donors with hypertension [17% vs 32%, p=0.035], diabetes [2% vs 11%, p=0.057], or death from cerebrovascular event (21% vs 36%, p=0.042). Higher KDPI was associated with decreased risk for PTE [HR 0.98 (95% CI: 0.97-0.99)]. Recipients of kidneys with KDPI ≥50% were less likely to develop PTE [HR 0.42 (0.22-0.79)] (Figure 1). Recipients with PTE were more likely to receive an angiotensin converting enzyme inhibitor or angiotensin receptor blocker (ACEi/ARB) compared to those without PTE during the 5 year follow up [66% vs 34%, p<0.001]. Only 17 (36%) recipients with PTE continued to have elevated Hb above PTE definition threshold during follow-up. There was no association of PTE with graft failure or mortality
*Conclusions: PTE among deceased-donor KTx recipients in this multi-center cohort was lower compared to prior published reports and resolved in most cases. Recipients of lower KDPI kidneys were at greater risk for PTE. Around a third of KTx recipients with PTE did not receive ACEi/ARB’s and this potential under-utilization should be explored in future studies
To cite this abstract in AMA style:
Alasfar S, Jia Y, Hall IE, Philbrook HThiessen, Mansour SG, Doshi MD, Mohan S, Bromberg JS, Reese PP, Parikh C. Incidence and Risk Factors of Post-Transplant Erythrocytosis in Deceased Donor Kidney Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/incidence-and-risk-factors-of-post-transplant-erythrocytosis-in-deceased-donor-kidney-transplantation/. Accessed February 20, 2026.« Back to 2020 American Transplant Congress