In Clinic Systems to Address Adherence Barriers Decrease Late Allograft Rejection for Kidney Transplant Patients.
Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Meeting: 2017 American Transplant Congress
Abstract number: 360
Keywords: Immunosuppression, Rejection
Session Information
Session Name: Concurrent Session: Kidney: Pediatric Adherence and Allocation
Session Type: Concurrent Session
Date: Monday, May 1, 2017
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:42pm-4:54pm
Presentation Time: 4:42pm-4:54pm
Location: E353B
Background: Patient-identified barriers to taking immunosuppressive medications are associated with rejection and allograft loss in kidney transplant patients, yet interventions targeting adherence barriers are rarely integrated into clinical practice.
Objective: To decrease late rejection by improving immunosuppressant adherence through integrated in-clinic systems to address adherence barriers in pediatric and adolescent kidney transplant recipients.
Methods: Using the Model for Improvement and iterative Plan-Do-Study-Act cycles, we implemented key systems to identify and address barriers to adherence including: 1) pre-clinic automated screening for adherence risk using data from the electronic health record, 2) in-clinic assessment of 14 common barriers to adherence using a standardized checklist, 3) shared decision aids for barrier-specific, patient-centered interventions, and 4) optional electronic adherence monitoring. Using statistical process control, we performed prospective time series analysis of patient days between late rejections (PDBRs) using a G-chart. Baseline median and 3-sigma control limits were calculated for PDBRs from 1/2013- 1/2016 and carried forward for comparison after full implementation of the intervention bundle. Data points outside control limits were considered special cause indicating improvement in the system.
Results: There were 66 late rejections over 4 years. Baseline median PDBRs was 1,455 and the upper control limit was 8,391. Within 5 months of implementing all system components, we observed 10,472 PDBRs indicating special cause and an improved system. This translates to 7 fewer rejections than expected during this time and an estimated savings of $595,000 in hospital charges. Post intervention median PDBRs has increased by 45% to 2108. 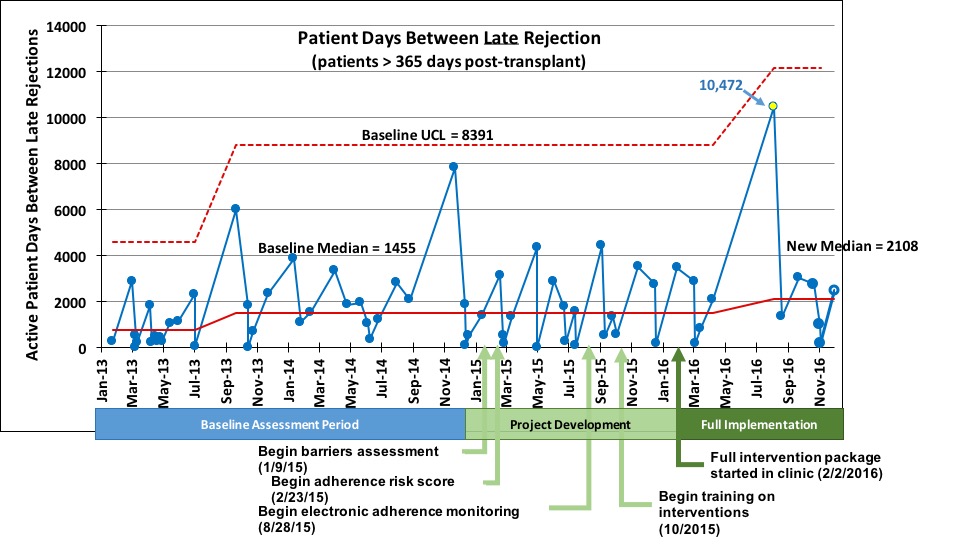 Conclusions: An integrated system to address adherence barriers in clinic was associated with reduced late rejections in pediatric and adolescent kidney transplant patients. This approach may also address adherence barriers in other transplant populations thereby improving health while reducing cost.
Conclusions: An integrated system to address adherence barriers in clinic was associated with reduced late rejections in pediatric and adolescent kidney transplant patients. This approach may also address adherence barriers in other transplant populations thereby improving health while reducing cost.
CITATION INFORMATION: Hooper D, Varnell, Jr. C, Rich K, Dahale D, Huber J, Pai A, Modi A. In Clinic Systems to Address Adherence Barriers Decrease Late Allograft Rejection for Kidney Transplant Patients. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Hooper D, Varnell C, Rich K, Dahale D, Huber J, Pai A, Modi A. In Clinic Systems to Address Adherence Barriers Decrease Late Allograft Rejection for Kidney Transplant Patients. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/in-clinic-systems-to-address-adherence-barriers-decrease-late-allograft-rejection-for-kidney-transplant-patients/. Accessed February 27, 2026.« Back to 2017 American Transplant Congress
